Outcome of Auditory Neuropathy Spectrum Disorder after Cochlear Implantation
Abdul Monem Al Shaikh,Hatem Ezz Eldin and Alaa Abusetta
DOI10.4172/2472-1786.100027
Sohag University, Sohag, Eygpt
- Corresponding Author:
- Hatem H Ezzeldin
Faculty of Medicine
Sohag University, Sohag, Eygpt
Tel: 00966594183458
E-mail: hezzm268@yahoo.com
Received date: January 27, 2016; Accepted date: May 12, 2016; Published date: May 19, 2016
Citation: Shaikh AMA, Eldin HE, Abusetta A. Outcome of Auditory Neuropathy Spectrum Disorder after Cochlear Implantation. J Child Dev Disord. 2016, 2:3.doi: 10.4172/2472-1786.100027
Abstract
Purpose: To record language and auditory skills development before and after cochlear implantation (CI) in children with Auditory neuropathy spectrum disorder (ANSD), and to determine the outcome after cochlear implant in patients with ANSD in comparison to patients with sensorineural hearing loss (SNHL).
Materials and methods: Cases Included in this study were divided into two groups. Group I: includes, 13 children diagnosed with ANSD, of them 7 cases were subjected to CI. Group II: includes, 20 cases of SNHL, of them 10 patients were subjected to cochlear implant. For all cases language therapy was given regularly for 6 months pre-operatively and 6 months post-operatively. Auditory Skills Checklist (ASC) and The Arabic language test (receptive, expressive and total language Quotients) were used to monitor the progress concerning auditory skills and language development.
Results: There was significant improvement in SNHL group and ANSD group after cochlear implantation regarding auditory skills (AS) and language development and almost the same outcome was obtained in both groups.
Conclusion: Cases with ANSD improved markedly after cochlear implantation and No differences were noticed in outcome between SNHL & ANSD groups.
Auditory neuropathy spectrum disorder (ANSD) is a hearing disorder characterized by normal functioning of outer hair cells, evidenced by intact cochlear microphonic (CM) potentials and Otoacoustic emissions (OAEs) with absent or severely desynchronized auditory brainstem response (ABRs) [1]. It is much more common than most investigators initially thought. Current incidence of ANSD is 0.5% to 1.3% of patients attending the audiology clinics [2].
They account about 12% to 14% of patients having absent ABR. The vast majority of the patients have absent ABR and Wave I is always absent, CM is Present in all cases of ANSD, OAEs may miss up to 50% of cases [1, 3]. ANSD may be caused by Hereditary, metabolic, toxic or inflammatory conditions. Hyperbilirubinemia, kernicterus and anoxia are possible factors [4].
Pathophysiology
Possible site of lesion
1) Inner hair cells (IHC) and auditory nerve dendrites.
2) Spiral ganglion, synaptic junction between IHC and auditory nerve.
(3) Auditory nerve axons (demyelinated, axonal degeneration).
Patients with AN may show poor temporal encoding and degradation of speech perception, ranging from limited to no open-set discrimination [5].
Clinical features
Starr et al. [1] reported that the patients may show varied SNHL mild to severe and usually bilateral.
Poor speech discrimination, absent or severely abnormal ABR may also be encountered. They also mentioned that hearing aids, FM systems, tactile aids are seldom of benefit.
The goals of present study
1. To explore development of auditory skills and language development before and after cochlear implantation in children with AN.
2. To compare the outcome after CI in points with AN Vs Pts. with SNHL.
Subjects and Methods
1. This study was conducted on children presented to ENT Center, King Fahd Hospital, Jeddah, from the period of April, 2010 to April, 2011 complaining of hearing impairment and delayed language development.
2. The Patients selected according to audiological evaluation (ABR- OAEs and Cochlear microphonic).
Total cases examined during the whole period 72. The number of cases with auditory neuropathy spectrum disorder was 13. The percentage of auditory neuropathy was about 18% of total cases diagnosed with Bilateral SNHL.
1. ALL cases were fitted with the proper hearing aids adjusted according to DSL i/o fitting formula (used regularly).
2. ANSD patients fitting followed a flexible way where loudness adaptation was taken into consideration.
Aided levels for all cases ranged between 50-60 dBHL. Cases Included in this study were divided into:
Group I: 13 children diagnosed with ANSD, 7 cases subjected to cochlear implant.
Group II: 20 cases of severe to profound or profound SNHL hearing loss, 10 patients subjected to cochlear implant.
For all cases language therapy was given in our center three sessions per week regularly for 6 months pre operatively and 6 months post operatively to monitor the progress concerning auditory skills and language development. We followed Auditory training rehabilitation program elaborated by Erber [6] and Ross [7]. They designed auditory training programs for rehabilitation of pre-lingual hearing impaired children which involve:
1. Sound detection
2. Sound discrimination
3. Sound identification
4. Sound recognition
5. Comprehension
Visual and auditory cues (lip-reading) are used in the beginning of the training with gradual removal of the visual cues. Then auditory cues only are used. The training rooms were quiet and furnished by carpets on the ground curtains on the walls to reduce noise for the optimal listening conditions. Noise makers and different materials were used to facilitate training sessions.
Phoniatric evaluation
Phoniatric Evaluation was done for all cases immediately after diagnosis, 6 months after language therapy and 6 months post cochlear implant.
Phoniatric evaluation includes
Auditory skills check-list (ASC) [8]
It measures the progress in various auditory skills. The check list consisted of 35 items representing 4 domains: detection (9 items), discrimination (7 items), identification (7 items), and comprehension (12 items). At the time of administration, each item of the scale was rated as one of the following: does not have skill, emerging skill, and developed skill. These levels of skill were then quantified respectively as 0, 1, or 2. The 35 questions on the ASC were quantified to yield a total possible raw score of 70, with a range of the total score to fail between 0 and 70 (detection=18 points, discrimination=14 points, identification=14 points, comprehension=24 points). Higher scores reflect higher or more developed functional auditory skills. Assessing Functional Auditory Skills in Young Children With Implants children who received a cochlear implant were expected to increase their ASC score by 8 points every 3 months.
The Arabic language test [9]
For monitoring the progress in different language parameters by calculating the Expressive Language Quotient (ELQ), Receptive Language Quotient (RLQ) and total language Quotient (TLQ).
Psychometric evaluation
Using (nonverbal Wechsler Intelligence Scale for Children) [10]. All children demonstrated at least normal range of non-verbal Intelligence Quotient (IQ ≥ 95).
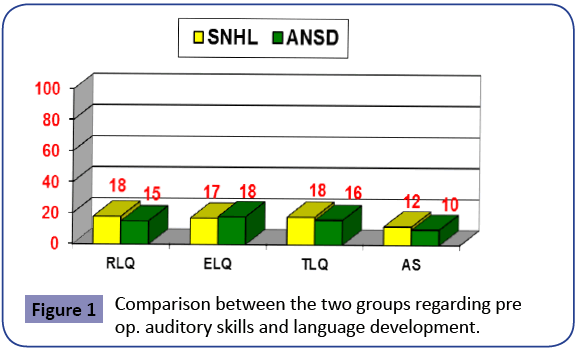
Children with ANSD were 6 boys (46%) and 7 girls (54%) with a mean age of 38 months ± 6 months. Children with SNHL were 10 boys (50%) and 10 girls (50%) with a mean age of 40 ± 8months. Children of both groups were similarly matched by age and IQ (Figure 1).
Statistics
Analytical statistics was done using Student’s “t” test to compare between two independent groups. Paired t-test used to compare means on the same subjects over time or in differing circumstances. Statistical significance was associated with a P value of less than 0.05 (Table 1).
| Variables | SNHL group | ANSD group | T-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | P. | Sign | |
| Chronological age (months) | 38±6 | 40 ± 8 | >0.05 | NS |
| gender Distribution (M:F) | M: 10 (50%) F: 10 (50%) |
6 (46%) 7 (54%) |
>0.05 | NS |
| IQ | 92.3 ±11 | 98.5 ± 8 | >0.05 | NS |
Table 1: Comparison between the SNHL group and ANSD group regarding the demographic data.
Results
Results of language assessment
Results of language therapy (6 ms) prep. for both groups
No statistical differences were found in both groups after 6 months of regular language therapy (Figure 2).
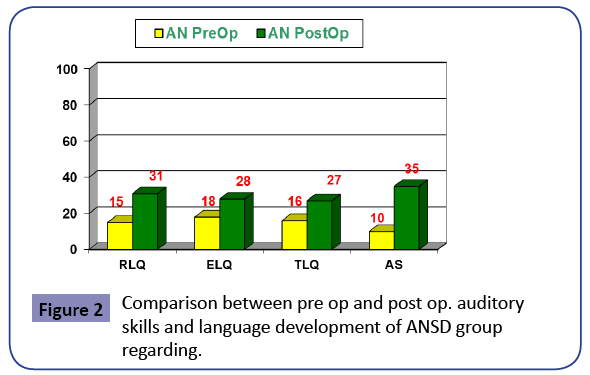
There was highly significant difference regarding auditory skills development. There was significant difference between pre-op. and post-op regarding different language parameters.
Six cases showed evident improvement concerning auditory skills and different language parameters after CI. One case showed little improvement compared to the other cases.
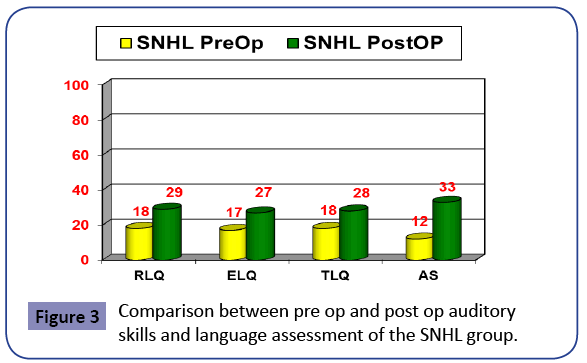
There was highly significant difference regarding auditory skills development. Pre op. and post op. and significant difference regarding different language parameters (Figure 3).
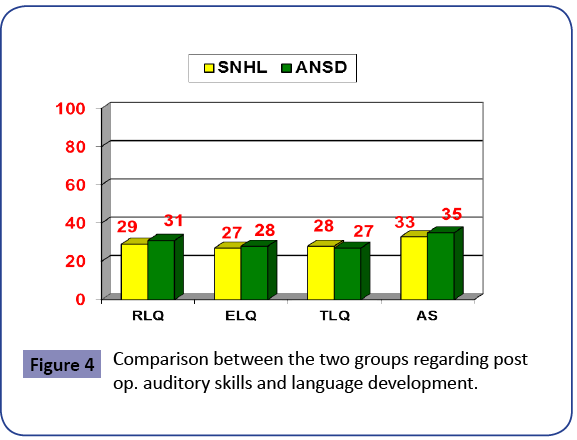
There was insignificant difference between SNHL group and ASND group regarding auditory skills development and different language parameters (Figure 4).
Discussion
Auditory neuropathy Spectrum Disorder is a challenging disorder and needs special rehabilitative approach. ANSD management aims at restoring the compromising processing of auditory information, either through conventional amplification and/or alternative forms of communication, or by cochlear implantation combined with intensive speech and language therapy.
In this study we found no benefit of H.As. and amplification for cases with ANSD, this coincide with the conclusion reached by Shallop et al. [11] who reported limited success with H-A, FM systems and tactile aids, as the problem of neural desynchrony is not addressed and even lead to a detrimental effect.
In this study 6 cases diagnosed with ANSD out of seven showed significant and satisfactory results after CI. They achieved more than 16 points in Auditory Skills Checklist (ASC) six months after auditory rehabilitation program. The results obtained because all candidates were young children and the lesion was mostly presynaptic, the inner hair cells within the synapses were the site of lesion and most of auditory nerve fibers are intact.
Shallop et al. [11] mentioned that their experiences with cochlear implantation for children diagnosed with ANSD have been very positive. All of the 5 children implanted have shown significant improvements in their sound detection, speech perception abilities and communication skills. All of the children have shown evidence of good NRT results postoperatively.
Teagle HB et al. [12] conducted study on 70 children who underwent CI. They mentioned that although 50% of the implanted children with ANSD demonstrated open-set speech perception abilities after implantation, nearly 30% of them with >6 months of implant experience were unable to participate in this type of testing because of their young age or developmental delays. Many of these children were born prematurely (42%) and impacted by a variety of medical comorbidities. More than one third (38%) had abnormal findings on preoperative magnetic resonance imaging of the brain and inner ear.
In this study one child failed to achieve significant improvement less than 16 points on Auditory Skills Checklist (ASC) six months after auditory rehabilitation program.
This may be explained by that children with ANSD who receive CIs are a heterogeneous group with a wide variety of impairments. Although many of these children may ultimately benefit from implantation, some will not, presumably because of a lack of electrical-induced neural synchronization, the detrimental effects of their other associated conditions, or a combination of factors.
Investigators [13-15] have shown that early cochlear implantation can be of benefit for some children with ANSD. In this study we found that most cases with AN improved markedly after CI concerning auditory skills and language development, this may be explained by the fact that electrical stimulation of the cochlea is better than acoustic stimulation for ANSD cases. Electric stimulation via a cochlear implant produced significantly higher intelligibility than acoustic stimulation. Simmons et al. [16] mentioned that CI promotes neural survival, restores temporal encoding, produces synchronous ABRs in the presence of peripheral nerve demyelination and they recommended CI for selected cases of ANSD.
Although the present results support cochlear implantation as one treatment choice for subjects with ANSD, success in implantation may depend on the site of the pathology.
In this study, no significant differences were noticed in outcome between SNHL & ANSD groups after Cochlear implant. Many authors proved benefit of subjects with SNHL after cochlear implantation. This can be understood under the notion that cochlear implant substitutes the function of the lost cochlear amplifier and transducer, namely outer hair cells. On the other hand, Participants with ANSD most likely derive the clear speech advantage from enhanced temporal fidelity and improved neural synchrony with electric stimulation.
Conclusion
1. Cases with ANSD improved markedly after cochlear implantation. We should elaborate about the choice of the cases with good thickness of the auditory nerve in MRI.
2. No significant differences were noticed in outcome between SNHL & ANSD groups.
Recommendations
1. Future study to examine the validity of the well-established protocol which includes waiting for 6 months preoperatively in AN cases.
2. More research work needed with big number of cases with long period of follow up.
References
- Starr A, Picton TW, Sininger Y, Hood LJ, Berlin CI, et al. (1996) Auditory neuropathy. Brain 119: 741-753.
- Tibesar RJ, Brissett AE, Shallop JK, Driscoll CL (2004) Internal auditory canal decompression and cochlear implantation in Camurati-Engelmann disease. Otolaryngol Head Neck Surg 131: 1004-1006.
- Rance G, Beer DE, Cone-Wesson B, Shepherd RK, Dowell RC, et al (1999) Clinical findings for a group of infants and young children with auditory neuropathy. Ear Hear 20: 238-252.
- Starr A, Sininger Y, Winter M, Derebery MJ, Oba S, et al. (1998) Transient deafness due to temperature-sensitive auditory neuropathy. Ear Hear 19:169-179.
- Berlin CI, Bordelon J, St John P, Wilensky D, Hurley A, et al. (1998) Reversing click polarity may uncover auditory neuropathy in infants. Ear Hear 19: 37-47.
- Erber N (1982)Auditory training. Washington, DC: Alexander Graham Bell Association for the Deaf.
- Ross M (2008) Listening to music through a cochlear implant. Hearing Loss 29: 20-23.
- Meinzen-Derr J, Wiley S, Creighton J, Choo D (2007) Auditory Skills Checklist: Clinical tool for monitoring functional auditory skill development in young children with cochlear implants. Ann OtolRhinolLaryngol 116: 812-818.
- Kotby MN, Khairy A, Barakah M, Rifaie N, EL-Shobary A, et al. (1995) Language testing of Arabic speaking children. Proceeding of the XVIII World Congress of the International Association of Logopedics and Phoniatrics, (WCIALP’95), Cairo, Egypt, pp: 263-266.
- Wechsler D (1991) Wechsler Intelligence Scale for Children. (3rd Eds) The Psychological Corporation, San Antonio.
- Shallop JK, Peterson A, Facer GW, Fabry LB, Driscoll CL, et al (2001) Cochlear implants in five cases of auditory neuropathy: postoperative findings and progress. Laryngoscope 111: 555-562.
- Teagle HF, Roush PA, Woodard JS, Hatch DR, Zdanski CJ, et al. (2010) Cochlear Implantation in Children with Auditory Neuropathy Spectrum Disorder. Ear Hear 31: 325-335.
- Zeng FG, Oba S, Garde S, Sininger Y, Starr A, et al (1999) Temporal and speech processing deficits in auditory neuropathy. Neuroreport 10: 3429-3435.
- Doyle KJ, Sininger Y, Starr A (1998) Auditory neuropathy in childhood. Laryngoscope 108: 1374-1377.
- Sheykholeslami K, Kaga K, Kaga M.J (2001) An isolated and sporadic auditory neuropathy (auditory nerve disease): report of five patients. LaryngolOtol 115: 530-534.
- Simmons JL, Beauchaine KL (2000) Auditory neuropathy: case study with hyperc bilirubinemia. J Am AcadAudiol 11: 337-347.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences