Is there an Autism "Epidemic" in the United States?
Michael Quinn1*, Brad Scott1 and Ryan J Hanson2
1Autism Support Now, LLC, Missouri, USA 2Froedtert Hospital, Milwaukee, Wisconsin, USA
Published Date: 2023-05-18DOI10.35841/2471-1786.9.3.62
Michael Quinn1*, Brad Scott1 and Ryan J Hanson2
1Autism Support Now, LLC, Missouri, USA
2Froedtert Hospital, Milwaukee, Wisconsin, USA
- *Corresponding Author:
- Michael Quinn
Autism Support Now, LLC, Missouri,
USA,
E-mail: mquinn@autismsupportnow.com
Received date: May 02, 2023, Manuscript No. IPCDD-23-16548; Editor assigned date: May 04, 2023, PreQC No. IPCDD-23-16548 (PQ); Reviewed date: May 10, 2023, QC No. IPCDD-23-16548; Revised date: May 12, 2023, Manuscript No. IPCDD-23-16548 (R); Published date: May 18, 2023, DOI: 10.35841/2471-1786.9.3.62
Citation: Quinn M, Scott B, Hanson RJ (2023) Is there an Autism “Epidemic” in the United States? J Child Dev Disord Vol.9 No. 3: 62.
Abstract
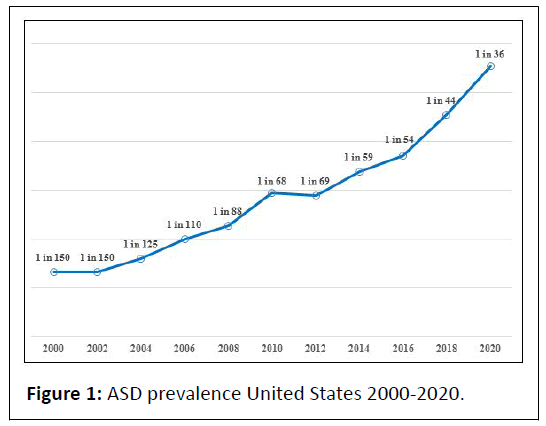
In the United States, according to recent research, Autism Spectrum Disorder (ASD) is one of the most prevalent neurodevelopmental disorders, affecting an estimated 1 in 36 children (approximately 4% of boys and 1% of girls). Since the Centers for Disease Control and prevention (CDC) first began tracking the disorder in 2000, the prevalence of ASD in children has risen by 316.7%. Consequently, the rise in the rate has sparked claims of an autism “epidemic”. However, the question remains are more children in the United States developing autism or is there simply a multitude of factors behind the rise in prevalence over time? The objectives of this paper are to explore the origins of the epidemic claims, outline potential explanations for the increasing prevalence and examine the economic implications. The main purpose of this paper is to provoke discussion among various stakeholders, particularly researchers and policymakers.
Keywords
Autism Spectrum Disorder (ASD); Children; Epidemic; Prevalence; United States
Introduction
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) [1], ASD is defined as a neurodevelopmental disorder characterized by persistent deficits in social communication, social interaction, and restricted, repetitive patterns of behavior. ASD signs and symptoms emerge in the first year of life and can be detected between 6 months and 18 months of age (CDC, 2023) [2]. Because autism manifests and impacts children and families differently, the DSM-5 includes three levels of support: Level 1 (“Requiring support”), Level 2 (“Requiring substantial support”) and Level 3 (“Requiring very substantial support”). Given that autism is a life-long impairment, considerable support is required to navigate different domains across the spectrum and throughout the lifespan (e.g., education, healthcare, peer relationships and/or employment). Since there is no medical test, like a blood test, to diagnose ASD, making a diagnosis may be difficult, because of the subjective nature of the diagnosis. However, several professionals, including physicians and clinical psychologists can diagnose ASD using behavioral criteria in accordance with diagnostic criteria outlined in DSM-5. Reports show that the average age of diagnosis is 4 years of age or older across North America (CDC, 2023). Autism is diagnosed based upon persistent deficits of social communication and interaction; restricted and repetitive behaviors, interests, activities. ASD is a heterogeneous disorder where each person has a distinct set of strengths and challenges. ASD is not a new phenomenon and has most likely existed since the origins of human society [3]. In 1943, Dr. Leo Kanner, an Austrian American child psychiatrist first described the core characteristics of ASD. During this period, Dr. Leo Kanner observed children who showed no interest in people or social interaction. Similarly, in 1944, Austrian pediatrician Hans Asperger coined the term Asperger syndrome after describing four young patients who had normal to high intelligence. However, these individuals manifested challenges in social interaction and expressed extremely narrow interests coupled with a tendency to be clumsy. While the etiology of ASD is multidimensional and complex [4], reports suggest a strong genetic basis [5-7]. Several other neurodevelopmental disorders are observed in autism [8] including intellectual disability, attention deficit hyperactivity disorder, specific motor and language disorders American Psychiatric Association, 2013. In 1996, the CDC began monitoring the prevalence of ASD, initially conducting studies among children in metropolitan Atlanta, Georgia [8]. In 2000, the Children’s Health Act [9] was enacted and authorized the CDC to establish the Autism and Developmental Disabilities Monitoring (ADDM) network. Since 2000, the CDC has supported biennial surveillance to track ASD prevalence in multiple communities. Currently, the ADDM network includes 11 sites (Arizona, Arkansas, California, Georgia, Maryland, Minnesota, Missouri, New Jersey, Tennessee, Utah and Wisconsin). Recently, the CDC reported that approximately 1 in every 36 children aged 8 years in the United States have been identified with ASD. The prevalence is approximately four times higher among boys than girls. Given the reported gender difference in prevalence, there are several possible explanations for the discrepancy in prevalence rates. For instance, previous research has reported that females camouflage ASD symptoms more than males, potentially contributing to the difference in prevalence [10]. Furthermore, there is evidence to suggest that females may be at a higher genetic threshold for ASD compared to males [11]. While the latest ADDM Network prevalence data represents large and diverse populations, they are not nationally representative and they rely on administrative records of developmental and/or educational assessments. Nevertheless, this paper will draw from the ADDM Network as it is frequently used as an indicator of ASD prevalence. With the significant rise in ASD prevalence, claims have been made we are experiencing an autism “epidemic”. Interestingly, the origins of these claims derive from laypersons who are unaware of the purposeful broadening of diagnostic criteria, coupled with greater public awareness and intentionally improved case finding. Furthermore, search autism “epidemic” online to witness the plethora of non-scientific articles endorsing an epidemic. ASD is surrounded by misperceptions and myths; even when scientifically disproven, these myths can be difficult to dispel [12]. Nevertheless, children diagnosed with autism need access to evidence-based support designed to alleviate symptoms and enhance developmental functioning. Recommended treatments include Applied Behavior Analysis (ABA) because it is a welldeveloped discipline, with a mature body of scientific knowledge, established standards for evidence-based practice and distinct methods of service delivery [13]. As the application of ABA therapy is advanced in practice, this scientific community gains further insights into detection, thereby decreasing the subjectivity of diagnosis.
Materials and Methods
ASD prevalence
There are three main measures of occurrence of a condition: Prevalence (the number of cases divided by the number of people in the population at a given time), incidence (the number of new cases among a given population in a defined time divided by the amount of person-time observed during the same period) and cumulative incidence (the number of new cases identified in an extended time period [e.g., from birth] divided by the size of the population without the disorder at the start of the time period) [14]. In the United States, estimates of ASD prevalence in children are collected through a variety of channels (e.g., the National Survey of Children’s Health, the United Sates Department of Education Special Education data and the CDC’s ADDM Network). While there are no perfect sources of data for evaluating ASD prevalence, as indicated earlier, this paper will draw from the ADDM Network as it is frequently used as an indicator of ASD prevalence. In 2023, the ADDM Network reported across 11 sites ASD prevalence per 1,000 children aged 8 years ranged from 21.1% in Maryland (1 in 43) to 44.9% in California (1 in 22). The overall prevalence was 27.6% per 1,000 (1 in 36) children aged 8 years in the United States, according to 2020 data (Table 1).
| Surveillance year | Birth year | Number of ADDM sites reporting | Year reported | Combined prevalence per 1,000 children | ASD prevalence rate |
|---|---|---|---|---|---|
| 2000 | 1992 | 6 | 2007 | 6.7 (4.5-9.9) | 1 in 150 |
| 2002 | 1994 | 14 | 2007 | 6.6 (3.3-10.6) | 1 in 150 |
| 2004 | 1996 | 8 | 2009 | 8 (4.6-9.8) | 1 in 125 |
| 2006 | 1998 | 11 | 2009 | 9 (4.2-12.1) | 1 in 110 |
| 2008 | 2000 | 14 | 2012 | 11.3 (4.8-21.2) | 1 in 88 |
| 2010 | 2002 | 11 | 2014 | 14.7 (5.7-21.9) | 1 in 68 |
| 2012 | 2004 | 11 | 2016 | 14.5 (8.2-24.6) | 1 in 69 |
| 2014 | 2006 | 11 | 2018 | 16.8 (13.1-29.3) | 1 in 59 |
| 2016 | 2008 | 11 | 2020 | 18.5 (18.0-19.1) | 1 in 54 |
| 2018 | 2010 | 11 | 2021 | 23 (16.5-38.9) | 1 in 44 |
| 2020 | 2012 | 11 | 2023 | 27.6 (23.1-44.9) | 1 in 36 |
| Note: ADDM network 2000-2020 combining data from all sites. | |||||
Table 1: Identified prevalence of Autism Spectrum Disorder (ASD).
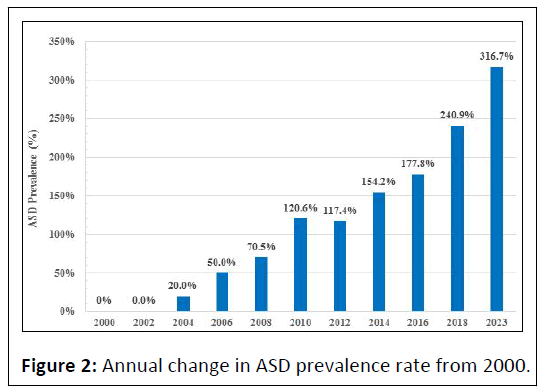
Interestingly and for the first time, rates were lowest for White children at 2.4% followed by 2.9% of Black children, 3.2% of Hispanic children and 3.3% of Asian/Pacific Islander children. Consequently, one could argue that screening and diagnosis has improved particularly in underserved communities. As mentioned, the prevalence is approximately four times higher among boys than girls. Interestingly, the latest ASD prevalence numbers, 1 in 36 shows a 316.7% increase from baseline numbers released in 2000, when the rate was 1 in 150 (Table 2).
| Year | 2000 | 2002 | 2004 | 2006 | 2008 | 2010 | 2012 | 2014 | 2016 | 2018 | 2020 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Annual rate | 0.70% | 0.70% | 0.80% | 1.00% | 1.10% | 1.50% | 1.40% | 1.70% | 1.90% | 2.30% | 2.80% |
| Relative difference from previous year | 0% | 0.00% | 20.00% | 25.00% | 13.60% | 29.40% | -1.40% | 16.90% | 9.30% | 22.70% | 22.20% |
| Annual change from 2000 | 0% | 0.00% | 20.00% | 50.00% | 70.50% | 120.60% | 117.40% | 154.20% | 177.80% | 240.90% | 316.70% |
Table 2: Annual change in ASD prevalence rate from 2000.
Results
As a result, this has fueled speculation that we are experiencing an autism “epidemic.” However, whether you are a proponent or skeptic of these claims, two fundamental questions are appropriate. Are more children in the United States developing autism or is there simply a multitude of factors behind the rise in prevalence over time? While it may be difficult to address these questions with a high degree of certainty, key stakeholders particularly policymakers and individuals in the field of epidemiology should remain cognizant of both genetic and non-genetic factors and how they alone or in combination, may impact the prevalence of ASD. Consequently, it could be argued that the bio-psychosocial approach may be the most appropriate conceptual model in understanding autism as a growing phenomenon.
This is because the bio-psychological perspective recognizes how biological, psychological and socio-cultural factors can influence human functioning [15,16]. As a result, this perspective lends itself to a much broader and integrated approach to intervention. This is something the medical model cannot achieve because it reflects a one-dimensional paradigm.
Figure 1 illustrates the rise in ASD prevalence from baseline numbers released in 2000 to the latest ADMM Network surveillance report. Table 2 outlines the annual percentage change in ASD prevalence rate from 2000.
Discussion
Origins of the epidemic claims
As reported, the CDC estimates that 1 in 36 8-year-old children have been identified with ASD, an increase from 1 in 150 children in 2000. As mentioned, these figures represent a 316.7% increase from baseline numbers released in 2000, when the rate was one in 150. Consequently, the rising prevalence of ASD has sparked claims of an autism “epidemic.” A logical place to start is to define the term “epidemic”. While the literature shows many definitions for the term, the simplest definition the authors found derived from the field of epidemiology. “If there are more cases than you expect, it’s an epidemic.” [12]. This definition provokes two important questions. For example, how many more cases must be recorded to constitute an epidemic? Whose expectations matter most? nevertheless, the term “epidemic” accentuates fear, a sense of danger and it is associated with a plague, consequently, having an impact on audiences and readers [12]. Interestingly and as previously outlined, much of the claims pertaining to the autism epidemic derive from laypersons who are unaware of the purposeful broadening of diagnostic criteria, coupled with greater public awareness and intentionally improved case finding [3]. Over the past decade, social media platforms have provided access to ASD information on an immeasurable scale. For instance, there is a plethora of online non-scientific articles referring to the rising cases of autism as an “epidemic”. For example, a large non-profit organization with 41-chapter locations in 50 states supporting individuals and families impacted by ASD recently stated in an online press release that a “prevalence of 1 in 36 cannot be disregarded. We cannot ignore this epidemic.” The same social media platforms have shared content claiming that autism is caused by vaccination. Yet, the scientific literature does not support an association of vaccination as an environmental factor that increases the risk for autism [17]. A large body of research has shown that there is no correlation between measles-mumps-rubella vaccine, mercury exposure by thimerosal-containing vaccines, aluminum in vaccines, or increased level of immunologic exposure attributable to a larger number of vaccines (either given at 1 time or cumulatively) with ASD [18-36]. However, there is an increasing number of parents choosing to withhold much-needed vaccinations for their children out of fear they will develop autism [12]. In many countries, vaccination rates have declined following the vaccineautism connection claims [37-39]. As a result, a significant proportion of children may be at risk for sudden illnesses. Apart from misinformation about autism, misinformation about the COVID-19 pandemic has also flourished on social media [40]. Social media companies have a moral duty to implement measures necessary to minimize the sharing of misinformation. For example, social media companies may consider establishing content moderation teams to mitigate the sharing of misinformation. Another suggestion is to direct users to other credible sources of information pertaining to ASD (e.g., American Academy of Pediatrics (AAP), Autism Speaks, CDC, National Institute of Health). However, because social media entities are privately-owned companies, they have the right to control what content is allowed and not allowed on their respective platforms. In the future, it is reasonable to assume that the federal government may at some stage attempt to enforce legislative reforms to curtail the spread of misinformation and conspiracy theories on social media platforms. However, the authors believe that such measures would simply exacerbate the issue and in the process, violate the first amendment of the United States Constitution. The United States Congress has also entered the discussion on the autism “epidemic”. For instance, several members have made claims on their respective .gov websites that America is facing an autism epidemic [3]. Yet, these claims are not supported by any scientific evidence and particularly concerning is they have been made by lawmakers who have the power to guide future public policies. Interestingly, a recent study demonstrated that lawmakers’ use of scientific evidence can be improved [41]. The authors of the paper argue that any political discourse and/or prospective laws pertaining to ASD and other major public health issues should be underpinned by science. In addition, several media headlines have surfaced perpetuating arguably a growing sense of fear. For example, there is a “mysterious upsurge” in ASD prevalence (New York Times, October 20, 2002, Section 4, p. 10) and new cases are “exploding in number” (Time, May 6, 2002, p.48) and “no one knows why” (USA today, May 17, 2004, p. 8D). To make an impact and be heard, politicians, journalists, philanthropic organizations and advocates use the word “epidemic” [12].
Potential explanations for increasing prevalence
Over the last decades, with steady increase in prevalence of ASD, the question arises about how much of this increase is real and how much of it is due to wider screening, broadening ASD diagnostic criteria, lower age of at diagnosis and intervention, a greater public awareness and parental advocacy [42]. There are several potential explanations for the increase in the observed prevalence of autism. For instance, there is increased public awareness of the disorder and its symptoms. In the new millennium, public and physician awareness of autism has increased markedly because of increased media coverage and a rapidly expanding body of knowledge published in professional journals [43]. Furthermore, a significant factor that may have led to increased reporting is celebrities making ASD awareness a cause due to an acquaintance or they themselves having an affected child [42]. Organizations have also played a significant role in raising awareness of ASD. For example, Autism Speaks Inc., a 501 (c) (3) nonprofit organization in the United States celebrates world autism month every April, beginning with the United Nations-sanctioned World Autism Awareness Day on April 2nd [44]. Throughout the month, Autism speaks coupled with other philanthropic organizations are focused on sharing stories and providing opportunities to increase understanding and acceptance of people with autism, fostering worldwide support. Apart from greater awareness, additional explanations for the rise in cases of autism may be that families are encouraged to test their children at a younger age. For instance, since 2007, universal screening has been recommended by the AAP for ASD at 18 and 24 months. Consequently, this may lead to earlier entry into intervention programs that support improved developmental outcomes. The AAP’s policy is significant because historically, the initial concerns of parents of children who later received diagnoses of ASD were dismissed and diagnosis and intervention were therefore delayed [45-48]. Research conducted in Atlanta, Georgia, found that the mean age for the first evaluation for 8-year-old children (n=115) with ASDs was 48 months and the mean age of the first ASD diagnosis was 61 months [49]. Although the AAP’s policy of universal screening for ASD in pediatric populations is encouraging, arguably the true prevalence of autism is still under-estimated. For instance, economic and socio-cultural factors are likely to perpetuate inequities in accessing healthcare for underserved communities. As a result, it is likely that there are a greater number of children at-risk for autism, but they may be missed or diagnosed late. Furthermore, research shows that compliance among primary care providers in screening ASD as recommended by the AAP is still not at 100% [50]. Are there are any other valid explanations? In 2013, the American Psychiatric Association merged four distinct autism diagnoses into one umbrella diagnosis of ASD. They included autistic disorder, childhood disintegrative disorder, Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) and Asperger syndrome [1]. This is significant because children who may have been historically diagnosed with other developmental disorders (e.g., mental retardation commonly referred to today as intellectual developmental disability) are now diagnosed with ASD. Additional factors such as policy changes may also be at play. Historically, many children with disabilities were denied access to education and opportunities to learn (U.S. Department of Education, 2023) [51]. However, under the Individuals with Disabilities Education Act (IDEA) (2004) [52], children with disabilities, including those with autism must be placed in the “least restrictive environment.” A “least restrictive environment” involves placing children in a setting where he/she has the greatest possible opportunity to interact with children who do not have a disability and to participate in the general education curriculum. Policymakers commonly refer to this approach as inclusive education. Under IDEA, schools are required to offer comprehensive evaluation for ASD and report to the United States Department of Education the annual number of children with disabilities, including autism who is being served in general classrooms. Interestingly, several argue that this data has been the most egregiously misused in arguments for an autism epidemic [3]. Scientists have argued that the increase in cases is due to more aggressive epidemiological methods that make it less challenging for researchers to count the correct number of cases [12]. What about the explanation that the rise in autism rates is due to the passing of insurance mandates across all fifty states? Interestingly, research has shown that after mandates were implemented after the first year, the prevalence of autism increased an average 10% [53]. Although the potential explanations for the rise in ASD prevalence are legitimate, no signal explanation by itself can account for the rise. As a result, key stakeholders, particularly policymakers should be cognizant of the multitude of factors that can influence human functioning.
Implications of rising ASD prevalence rates
As reported, the CDC estimates that the autism rate among 8- year-old children in the United States is 1 in 36, an increase from 1 in 150 children in 2000 [8]. The annual change in the ASD prevalence rate from 2000 represents a 316.7% increase (Figure 2).
Although it is not clear if more children in the United States are developing autism or if there is simply a multitude of factors behind the rise in prevalence, what is clear is that there are implications particularly of an economic nature. For example, from a healthcare perspective, researchers found that the utilization and costs of healthcare are significantly higher for children with ASD compared to their neurotypical peers. For instance, children on the spectrum engage more frequently with pediatricians, psychiatrists and neurologists compared to children without ASD [54]. The same research documented that children with ASD were nearly 9 times more likely to use psychotherapeutic medications and twice as likely to use gastrointestinal agents as children without ASD. Consequently, the demand for healthcare provisions wills likely increase if the prevalence of autism continues to grow as it has in recent years. Certainly, with the CDC expected to unveil new prevalence rates in 2023, one can assume costs will continue to rise. It is important to acknowledge that healthcare is only one area among many that has significant costs relevant to children with autism. Special education is another element of cost associated with this heterogeneous population. IDEA specifies that children with various disabilities, including autism, are entitled to early intervention services and special education. Similarly to healthcare, the demand for special education services coupled with associated costs will likely increase if we continue to observe an increase in ASD prevalence. For example, in California, over $12 billion in state, federal and local funds each year is allocated to provide special education and related services [55]. This level of funding is significant and because the rate of ASD per 1,000 children is higher in California (44.9%) compared to other CDC sites (e.g., Maryland, 21.1%), a sustained effort from stakeholders is necessary to ensure students with autism continue to receive school-based supports needed to succeed in school and in the community. On a national level, reports suggest that the total annual costs of caring for American children with autism may exceed 589 billion dollars by 2030 [56]. Consequently, this figure highlights the need for stakeholders, particularly policymakers at a state and federal level to adopt prudent economic policies.
Conclusion
This paper explored the origins of the epidemic claims, outlined potential explanations for the increasing prevalence and examined the economic implications. The authors of this paper argue that there is no autism “epidemic” but rather a multitude of factors behind the rise in prevalence, which in no way diminishes the importance of addressing ASD as a major public health issue. As outlined, these factors included greater public awareness and advocacy, the introduction of universal screening, broadening of ASD diagnostic criteria, a policy of inclusive education and the passing of insurance mandates. Interestingly, there is zero discussion on the CDC website about the observed increase in ASD prevalence representing an “epidemic”. If we are to believe that there is an autism “epidemic” in the United States, shouldn’t we expect the CDC, a leading authority on autism and other neurodevelopmental conditions to declare that this is the case? Lastly, there is a need for stakeholders, particularly policymakers, to address the rising rate of ASD as more than a major public health issue but rather an opportunity to implement policies that promote additional investment in early intervention services. As a result, this could lead to substantial potential savings for federal and state governments. For example, early intervention for children with ASD can increase independence at home, at school and in the community. Consequently, improving the quality of life and decreasing the level of dependency on state and federal resources.
References
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: American Psychiatric Association.
[Crossref], [Google Scholar]
- Centers for Disease Control and Prevention (2023) Autism Spectrum Disorder (ASD).
- Gernsbacher MA, Dawson M, Goldsmith HH (2005) Three reasons not to believe in an autism epidemic. Curr Dir Psychol Sci 14: 55-58.
[Crossref], [Google Scholar], [Indexed]
- Quinn M, Strothkamp T, Seper-Roper A (2018) Supporting children with autism using an evidence-based approach. J Child Dev Disord 4: 1-3.
[Crossref], [Google Scholar]
- Rylaarsdam L, Guemez-Gamboa A (2019) Genetic causes and modifiers of autism spectrum disorder. Front Cell Neurosci 13: 1-15.
[Crossref], [Google Scholar], [Indexed]
- Persico AM, Napolioni V (2013) Autism genetics. Behav Brain Res 251: 95-112
[Crossref], [Google Scholar], [Indexed]
- Geschwind DH (2011) Genetics of autism spectrum disorders. Trends Cogn Sci 15: 409-416.
[Crossref], [Google Scholar], [Indexed]
- Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, et al. (2021) Prevalence and characteristics of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ 70: 1-16.
[Crossref], [Google Scholar], [Indexed]
- Children’s Health Act (2000).
- Schuck RK, Flores RE, Fung LL (2019)Brief report: Sex/gender differences in symptomology and camouflaging in adults with autism spectrum disorder. J Autism Dev Disord 49: 2597-2604.
[Crossref], [Google Scholar], [Indexed]
- Ratto AB, Kenworthy L,Yerys BE, Bascom J, Wieckowski AT, et al. (2018) What about the girls? sex-based differences in autistic traits and adaptive skills. J Autism Dev Disord 48: 1698-1711.
[Crossref], [Google Scholar], [Indexed]
- Grinker RR (2008) Unstrange minds: Remapping the world of autism. Basic Books, Philadelphia.
- The Council for Autism Service Providers (CASP) (2014) Applied behavior analysis treatment of autism spectrum disorder: Practice guidelines for healthcare funders and managers. (2nd ed), CASP, Boston, MA.
- Rice CE, Rosanoff M, Dawson G, Durkin MS, Croen LS, et al. (2012) Evaluating changes in the prevalence of the Autism Spectrum Disorders (ASDs). Public Health Rev 34: 1-22.
[Crossref], [Google Scholar], [Indexed]
- Bronfenbrenner U (1979) The ecology of human development: Experiments by nature and design. Harvard University Press, Cambridge.
- Engel GL (1977) The need for a new medical model: A challenge for biomedicine. Science 196: 129-36.
[Crossref], [Google Scholar], [Indexed]
- Hyman SL, Levy SE, Myers SM, Kuo D, Apkon S, et al. (2020) APP council on children with disabilities, section on developmental and behavioral pediatrics. Executive summary: Identification, evaluation and management of children with autism spectrum disorder. Pediatrics 145: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Kalkbrenner AE, Schmidt RJ, Penlesky AC (2014) Environmental chemical exposures and autism spectrum disorders: A review of the epidemiological evidence. Curr Probl Pediatr Adolesc Health Care 44: 277-318.
[Crossref], [Google Scholar], [Indexed]
- Jain A, Marshall J, Buikema A, Bancroft T, Kelly JP, et al. (2015) Autism occurrence by MMR vaccine status among US children with older siblings with and without autism. Jama 313: 1534-1540.
[Crossref], [Google Scholar], [Indexed]
- Uno Y, Uchiyama T, Kurosawa M, Aleksic B, Ozaki N, et al. (2015) Early exposure to the combined measles–mumps–rubella vaccine and thimerosal-containing vaccines and risk of autism spectrum disorder. Vaccine 33: 2511-2516.
[Crossref], [Google Scholar], [Indexed]
- Taylor LE, Swerdfeger AL, Eslick GD (2014) Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine 32: 3623-3629.
[Crossref], [Google Scholar], [Indexed]
- Maglione MA, Das L, Raaen L, Smith A, Chari R, et al. (2014) Safety of vaccines used for routine immunization of US children: A systematic review. Pediatrics 134: 325-337.
[Crossref], [Google Scholar], [Indexed]
- DeStefano F, Price CS, Weintraub ES (2013) Increasing exposure to antibody-stimulating proteins and polysaccharides in vaccines is not associated with risk of autism. J Pediatr 163: 561-567.
[Crossref], [Google Scholar], [Indexed]
- Demicheli V, Rivetti A, Debalini MG, Pietrantonj CD, et al. (2013). Vaccines for measles, mumps and rubella in children. Evidence-Based Child Health: A Cochrane Review Journal 8: 2076-2238.
[Crossref], [Google Scholar], [Indexed]
- Örtqvist Å, Blennow M, Carlsson RM, Hanson LÅ, Lindberg A, et al. (2010) Vaccination of children–a systematic review. Acta Paediatr 99: 1.
[Crossref], [Google Scholar], [Indexed]
- Gerber J, Offit PA, Plotkin S (2009) Vaccines and autism: A tale of shifting hypotheses. Clin Infect Dis 48: 456-6l.
[Crossref], [Google Scholar], [Indexed]
- Schechter R, Grether JK (2008) Continuing increases in autism reported to California's developmental services system: Mercury in retrograde. Arch Gen Psychiatry 65: 19-24.
[Crossref], [Google Scholar], [Indexed]
- Kimmel SR, Burns IT, Wolfe RM, Zimmerman RK (2007) Addressing immunization barriers, benefits and risks. J Fam Pract 56: S61-S65.
[Google Scholar], [Indexed]
- Baird G, Pickles A, Simonoff E, Charman T, Sullivan P, et al. (2008) Measles vaccination and antibody response in autism spectrum disorders. Arch Dis Child 93: 832-837.
[Crossref], [Google Scholar], [Indexed]
- Fombonne E, Zakarian R, Bennett A, Meng L, McLean-Heywood D, et al. (2006) Pervasive developmental disorders in Montreal, Quebec, Canada: Prevalence and links with immunizations. Pediatrics 118: 139-150.
[Crossref], [Google Scholar], [Indexed]
- Mutter J, Naumann J, Schneider R, Walach H, Haley B, et al. (2005) Mercury and autism: Accelerating evidence? Neuro Endocrinol Lett 26: 439-446.
[Google Scholar], [Indexed]
- Parker SK, Schwartz B, Todd J, Pickering LK (2004) Thimerosal-containing vaccines and autistic spectrum disorder: A critical review of published original data. Pediatrics 114: 793-804.
[Crossref], [Google Scholar], [Indexed]
- Institute of Medicine Immunization Safety Review Committee (2004) Immunization safety review: Vaccines and autism. National Academies Press, Washington, DC.
[Crossref], [Google Scholar], [Indexed]
- Jefferson T, Price D, Demicheli V, Bianco E (2003) European research program for improved vaccine safety surveillance project. Unintended events following immunization with MMR: A systematic review. Vaccine 21: 3954-3960.
[Crossref], [Google Scholar], [Indexed]
- Klein KC, Diehl EB (2004) Relationship between MMR vaccine and autism. Ann Pharmacother 38: 1297-1300.
[Crossref], [Google Scholar], [Indexed]
- Wilson K, Mills E, Ross C, McGowan J, Jadad A, et al. (2003) Association of autistic spectrum disorder and the measles, mumps and rubella vaccine: A systematic review of current epidemiological evidence. Arch Pediatr Adolesc Med 157: 628-634.
[Crossref], [Google Scholar], [Indexed]
- Staten Serum Institute (2023) No association between MMR vaccine and autism.
- Hansen SN, Schendel DE, Parner ET (2015) Explaining the increase in the prevalence of autism spectrum disorders: Proportion attributable to changes in reporting practices. JAMA Pediatrics 169: 56–62.
[Crossref], [Google Scholar], [Indexed]
- McIntyre P, Leask J (2008) Improving uptake of MMR vaccine. BMJ 336: 729-730.
[Crossref], [Google Scholar], [Indexed]
- Pennycook G, McPhetres J, Zang Y, Lu JG, Rand DG, et al. (2020) Fighting COVID-19 misinformation on social media: Experimental evidence for a scalable accuracy-nudge intervention. Psychol Sci 31: 770-780.
[Crossref], [Google Scholar], [Indexed]
- Crowley DM, Scott JT, Long EC, Green L, Isreal A, et al. (2020) Lawmakers’ use of scientific evidence can be improved. PNAS 118: 1-5.
[Crossref], [Google Scholar], [Indexed]
- Neggers YH (2014) Increasing prevalence, changes in diagnostic criteria and nutritional risk factors for autism spectrum disorders. ISRN Nutrs 2014: 514026.
[Crossref], [Google Scholar], [Indexed]
- Johnson CP, Myers SM (2007) Identification and evaluation of children with autism spectrum Disorders. Pediatrics 120: 1183-1215.
[Crossref], [Google Scholar], [Indexed]
- Autism speaks (2023) World autism awareness day.
- Howlin P, Moore A (1997) Diagnosis in autism: A survey of over 1200 patients in the UK. Autism 1: 135-162.
[Crossref], [Google Scholar]
- Howlin P, Asgharian A (1999) The diagnosis of autism and Asperger syndrome: Findings from a survey of 770 families. Dev Med Child Neurol 41: 834–839.
[Crossref], [Google Scholar], [Indexed]
- Frith U, Soares I (1993) Research into earliest detectable signs of autism: What parents say. Communication 27: 17-18
- Siegel B, Pliner C, Eschler J, Glen E (1988) How children with autism are diagnosed: Difficulties in identification of children with multiple developmental delays. J Dev Behav Pediatr 9: 199-204. [Crossref],
[Google Scholar], [Indexed]
- Wiggins LD, Baio J, Rice C (2006) Examination of the time between first evaluation and first autism spectrum diagnosis in a population-based sample. J Dev Behav Pediatr 27: 79-87.
[Crossref], [Google Scholar], [Indexed]
- Daniels AM, Mandell DS (2013) Children’s compliance with American Academy of Pediatrics’ well-child care visit guidelines and the early detection of autism. J Autism Dev Disord 43: 2844-2854.
[Crossref], [Google Scholar], [Indexed]
- U.S. Department of Education (2023) A history of Individuals with Disabilities Education Act.
- Section 1400 (2004) The individuals with Disabilities Education Act.
- Mandell DS, Barry CL, Marcus SC, Xie M, Shea K, et al. (2016) Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatr 170: 887-893.
[Crossref], [Google Scholar], [Indexed]
- Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P, et al. (2006) A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics 118: 1203-1211.
[Crossref], [Google Scholar], [Indexed]
- Doutre S, Willis J, Barrett T, Ripma T, Caparas R, et al. (2021) California state special education funding system study, part 2. WestEd, California.
- Blaxill M, Rogers T, Nevison C (2021) Autism tsunami: The impact of rising prevalence on the societal cost of autism in the United States. J Autism Dev Disord 52: 2627-2643.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences