ADHD and the Generalizability of Treatment: A Survey of Community Professionals
Alexandra V Moreland1*, Ara Anspikian2, Sydney Young3, Denise Tran4, Andrew Minoru Fukuda5,6, Harinder Kaur Dhillon1,4, Bhaktidevi M. Rawal7, Jenae Torres1, Miguel Serrano Illan8, Carvy Floyd Luceno9 and Bianca Rebolledo1
1Loma Linda University Behavioral Medicine Center, Redlands, CA, USA
2Department of Psychiatry, Loma Linda University School of Medicine, Loma Linda, USA
3Mountain Vista Psychology, Englewood, USA
4Department of Psychiatry and Behavioral Sciences, University of Southern California, Los Angeles, USA
5Butler Hospital TMS Clinic and Neuromodulation Research Facility, RI, USA
6Department of Psychiatry and Human Behavior, Brown University, Alpert Medical School, RI, USA
7Department of Psychology, Loma Linda University, Loma Linda, USA
8Loma Linda University Medical Center, Loma Linda, USA
9Loma Linda University, School of Medicine, Loma Linda, CA, USA
*Corresponding Author:
- Alexandra V Moreland
- Loma Linda University Behavioral Medicine Center, Redlands, USA,
- E-mail: amoreland@llu.edu
Received date: October 07, 2022, Manuscript No. IPCDD-22-14812; Editor assigned date: October 10, 2022, PreQC No. IPCDD-22-14812 (PQ); Reviewed date: October 21, 2022, QC No. IPCDD-22-14812; Revised date: October 31, 2022, Manuscript No. IPCDD-22-14812 (R); Published date: January 31, 2023, DOI: 10.35841/2471-1786.9.1.43
Citation: Moreland AV, Anspikian A, Young S, Tran D, Fukuda AM, et al. (2022) ADHD and the Generalizability of Treatment: A Survey of Community Professionals. J Child Dev Disord Vol.9 No. 1: 43.
Abstract
Objective: The prevalence of ADHD among youth necessitates delivery of Evidence-Based Treatments (EBTs), but limited treatment generalizability to varied settings is a significant barrier. Disseminating knowledge and training to clinicians can assist with maintaining clinical gains for providers and continued improvement for youth with ADHD. The aim of this study is to explore how continued education and training on ADHD affects clinician’s understanding, barriers, and perceived ability to generalize treatment results across multiple settings.
Methods: Participants (N=70) were recruited from an ADHD conference at Loma Linda University Behavioral Medicine Center and administered pre and post surveys. Paired samples t-tests were used to evaluate pre and post conference responses.
Result: Results for 6 out of the 9 domains demonstrated statistical significance on post surveys indicating that the conference successfully improved clinician’s perceived ability to implement and generalize treatments to these settings; however, did not improve perceived barriers.
Conclusion: Continuing education and training can increase professionals’ knowledge and confidence of service delivery for ADHD and generalization effects throughout various treatment settings potentially leading to improved patient care for this vulnerable population.
Keywords: ADHD; Generalization; Evidence-based interventions; Children; Professionals; Continuing education
Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by chronic and pervasive difficulties with inattention, hyperactivity, and impulsivity that are disproportionate to age and development [1]. The onset of ADHD typically occurs in childhood and often persists into adolescence and adulthood with an estimated worldwide ADHD prevalence rate of 5% and prevalence rate of 8.8% in the United States. Among children and adolescents [2,3]. The two most utilized categories of evidence-based interventions are pharmacological and psychosocial interventions [4]. With well-established approaches to mitigating core features of ADHD.
However, the importance of generalization of ADHD treatment is underestimated and overlooked in current ADHD treatment practices. Generalization of ADHD treatment outcomes involves the child’s ability to complete a task, perform an activity, or display a behavior across multiple settings among different people and at different times. Success of generalization effects allows children to manage behaviors that negatively impact social, occupation and academic functioning ultimately enhancing treatment outcomes. Researchers and clinicians have identified two key components for successful generalization implementation: 1. Determine what kind of trainings and interventions best promote generalization gains and 2. Develop and implement effective training programs and assess factors contributing to generalization [5]. This study seeks to assess specific factors contributing to the implementation of generalizing ADHD treatment.
Pharmacological interventions
Guidelines of the American Academy of Child and Adolescent Psychiatry (AACAP) endorse stimulant medications as first-line treatment to improve ADHD symptoms; with demonstrated improvement of attention, focus, goal directed behavior and organizational skills [6,7]. Stimulant medications are often effective in reducing core ADHD symptoms (e.g., impulsivity, hyperactivity, inattention) and in increasing aspects of classroom functioning and academic productivity (e.g., classroom behavior, note-taking, scores on quizzes/worksheets, homework completion). Other medications such as guanfacine, clonidine, and some anti-depressants may also be helpful. The American Academy of Pediatrics recommends FDA-approved medication be used for the treatment of core ADHD symptoms for children 6 years of age and older [1].
Psychosocial interventions
Evidence-based psychosocial treatments for children and adolescents include cognitive skills training (i.e., executive functioning skills training, organizational skills training) and behavior modification (i.e., contingency management, behavioral parent training, behavioral peer intervention, behavioral classroom management) [8]. The efficacy of evidence-based psychosocial interventions is established in the literature and has become particularly more robust over the past decade. Psychosocial interventions demonstrate improvement in the home and school functioning of children with ADHD across various study designs and treatment settings (e.g., home, school, recreational) [9,10]. However, while most evidencebased treatments demonstrate efficacy in reducing core ADHD symptoms in the treatment settings, generalization of positive effects to non-treatment settings is highly variable [11] with limited literature discussing generalizability and ADHD.
Various psychosocial interventions such as behavioral parent training, organizational skills training, school-based accommodations, have demonstrated the ability to generalize skills to settings other than the primary treatment focus [10]. Specifically, parent-child interaction therapy, a form of behavioral parenting recommended by the American Academy of Pediatrics, showed treatment gains lasting 3 to 6 years post treatment with improvement with school engagement, social relationships, and comorbid internalizing and externalizing symptoms [12]. Organizational skills training, which addresses tracking assignments, managing material, time management and task planning shows treatment gains continue into the following school year and demonstrated organization skills functioning improved significantly in the home environment as well [13].
Although some psychosocial interventions demonstrate promising results of generalization, several psychosocial interventions (i.e. neurofeedback, mindfulness and cognitive training) have shown limited generalization effects [9,14,15] with therapeutic gains diminishing once treatment is withdrawn. Lastly, important factors that may influence the use of evidencebased practices are social perceptions (e.g., like/dislike, perceived effectiveness, anticipated stigma) of affected youth, their parents, health care professionals, and teachers regarding treatment acceptability and treatment-related risks and benefits [16]. Although certain psychosocial interventions have demonstrated greater likelihood to generalize to non-treatment settings, current research does not demonstrate sustained maintenance of treatment-related behavioral changes beyond 24 months of therapy.
Generalization of ADHD treatment
Effective generalization should occur in three forms; across settings (classroom, home, peer groups), across symptom domains (inattention, hyperactivity, impulsivity, oppositional, aggressive, or uncooperative behavior, impaired peer, and parent relationships), and across time [17]. The importance of the generalization and transfer of skills is underestimated and overlooked in current ADHD treatment practices. Existing research suggested that domain, setting and treatment intensity may overlap and interact therefore making treatment responses impossible to predict which leads to increasing the barriers to effective generalization [5]. This ultimately highlights the significant need for clinicians to have the tools and knowledge to further assist this population in facilitating generalization of treatment.
Professionals working in an intensive outpatient ADHD treatment program at Loma Linda University Behavioral Medicine Center developed an ADHD conference to provide information to medical, school-based and community professionals who work with the ADHD population regularly. The purpose of developing this ADHD conference was to examine how continued education and training in ADHD treatment will affect local clinicians’ and community professionals perceived ability and confidence in implementing treatments and addressing perceived barriers to ADHD treatment. In this paper, we explore how continued education and training on ADHD and evidence-based treatments of ADHD affected clinician’s perceived ability to implement treatments, their perceived barriers to implementation of treatment and perceived ability to generalize treatment results across multiple settings.
Methods
Objectives
The aim of this study was to explore how continued education and training on ADHD and evidence-based treatments of ADHD affects medical, school and community-based professionals:
1. Perceived ability to implement evidence-based treatments for ADHD.
2. Perceived barriers to implement evidence-based treatments for ADHD.
3. Perceived ability to generalize treatment outcomes across multiple settings.
Hypothesis Professionals who attend the ADHD continuing education conference will indicate an increase in their confidence, training, and support of evidence-based treatment approaches for ADHD.
Participants
Participants represented a range of medical and school-based professionals that work with children diagnosed with ADHD including teachers (n=9, 13%), nurses (n=23, 33%), school psychologists (n=4, 6%), mental health clinicians (psychologists, MFT, LCSW, LPCC) (n=18, 6%), social workers (n=6, 9%), speech and language therapists (n=2, 3%), and other (e.g.: Mothers) (n=8, 11%). Participants were recruited from an eight-hour ADHD didactic, “A-Z’s of ADHD” conference at the Institution. All participants were at least 18 years old. Participant’s years of exposure working with the ADHD population ranges from 0 to 40 years. A total of 4 participants did not provide their years of experience. See Table 1 for participant demographics.
Table 1: Participant demographics, Percentages of demographic data collected (age, gender profession, experience) for conference attendees.
| Participant Demographics (N = 70) | ||
|---|---|---|
| n | (%)* | |
| Age | ||
| 18-24 | 1 | 1% |
| 25-34 | 9 | 13% |
| 35-44 | 19 | 27% |
| 45-54 | 19 | 27% |
| 55-64 | 18 | 25% |
| 65-74 | 3 | 4% |
| 75+ | 1 | 1% |
| Gender | ||
| Male | 5 | 7% |
| Female | 48 | 69% |
| Unanswered | 17 | 24% |
| Profession | ||
| Teacher | 9 | 13% |
| Nurse | 23 | 33% |
| School Psychologist | 4 | 6% |
| Therapist (Psychologist, MFT, LCSW, LPCC) | 18 | 25% |
| Social Worker | 6 | 9% |
| Speech & Language | 2 | 3% |
| Other | 8 | 11% |
| Years of exposure to ADHD Children | ||
| 0 to 10 | 31 | 44% |
| 11 to 20 | 22 | 31% |
| 21 to 30 | 9 | 13% |
| 31 to 40 | 5 | 7% |
| Unanswered | 3 | 4% |
| Note: Number of participants varies slightly in tables of result because participants did not always answer questions fully *Percentages rounded to nearest whole number |
||
Conference survey
The conference was designed and presented by therapists (LPCC, LMFT) and psychiatrists working within the intensive outpatient child and adolescent ADHD program at the Institution. The conference examined the epidemiology, diagnosis, assessment and best practice modalities for ADHD. Materials and presentations included informative handouts, presentations, and hands-on activities intended to enhance participants’ confidence in their knowledge about working with children with ADHD. The total duration of the conference was eight hours.
The information provided at the conference was presented in accordance with the following 12 objectives: (1) improve knowledge and understanding of evidence-based psychological assessments for ADHD, (2) review objective information regarding the relationship between diet and mental health along with dietary recommendations for optimal mental health, (3) review the physiological pathways and mechanisms of inflammation as they relate to diet and mental health, (4) utilize skills and interventions from Parent Management Training to manage ADHD symptoms and disruptive behaviors, (5) improve knowledge and understanding of evidence-based psychosocial interventions for the treatment of ADHD in children and families, (6) obtain an understanding of special education services and how children with ADHD and their families can benefit, (7) describe the basic neurobiological foundations of ADHD, (8) describe the general categories and effectiveness of medication used to treat ADHD, (9) learn about the differential diagnoses of ADHD, (10) increase knowledge and stimulate questions related to ADHD treatment generalization, (11) identify characteristics of executive functioning and social skills deficits in children with ADHD, and (12) identify strategies to improve social skills and executive functioning in children with ADHD.
Development of ADHD research survey
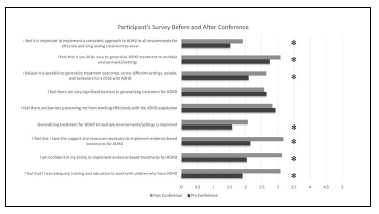
The investigators developed a survey to assess participants’ perceived ability and confidence in implementing treatments and managing perceived barriers to ADHD treatment. Survey items used in this study were based on clinical experience and a review of the current literature exploring ADHD perceptions and generalizability. Beyond demographic data collected from participants, each pre- and post-survey included nine statements related to the three objectives of the study discussed prior (Figure 1).
Procedure
This cross-sectional study used the pre and post survey method to answer the research questions. Ethical approval for the study was obtained from Loma Linda University Health Internal Review Board (IRB #5170109) and standard procedures to ensure human subjects protection were implemented throughout the study. Upon arriving at the conference, each participant was provided with an informed consent form, which was verbally reviewed by a research assistant and addressed participants’ questions or concerns. Each participant was administered the survey twice-once at the beginning of the conference and once at the conclusion of the conference for pre- and post-conference data, respectively. Both the pre and post conference surveys took approximately 15 minutes to complete. There was no incentive to complete the pre and post conference survey.
Data analysis
Descriptive statistics were computed for frequencies and percentages for demographic information (age, gender, profession, and years of exposure to ADHD children) including frequencies, percentages, means, standard deviations. Pre and post conference surveys were analyzed with a paired samples ttest. Outcomes from analysis compared differences between participants’ perceived ability to implement ADHD treatments, perceived barriers to implement treatment, and perceived ability to generalize treatments before and after the ADHD training conference (Table 2). A p-value <0.05 was considered statistically significant. Data analysis was performed with SPSS version 27 statistical software. P values of <0.05 were considered statistically significant.
Results
Of the 70 participants, all 70 completed the initial demographic data. However, for the 9 domains evaluated on the survey, only 47 participants (67%) completed both pre and post surveys. Demographic data are presented in Table 1. Results for 6 out of the 9 domains evaluated demonstrated statistically significant changes on pre and post surveys with p-values < 0.05. Survey components and domains are presented in Table 2.
Table 2: Pre and Post Survey Outcomes. Outcomes of survey questions based on pre and post data collection. Results for 6 out of the 9 domains demonstrated statistical significance on post surveys.
|
|
Pre-test | Post-test | |
|---|---|---|---|
|
|
Mean (SD) n=47 | M (SD) n=47 | p |
| Question 1 I feel that I have adequate training and education to work with children who have ADHD |
3.08 (1.08) | 1.89 (.84) | .000* |
| Question 2 I am confident in my ability to implement evidence-based treatments for ADHD |
3.12 (1.01) | 2.02 (.76) | .000* |
| Question 3 I feel that I have the support and resources necessary to implement evidence-based treatments for ADHD |
3.17 (1.00) | 2.12 (.84) | .000* |
| Question 4 Generalizing treatment for ADHD to multiple settings is important |
2.06 (1.00) | 1.57 (.85) | .004** |
| Question 5 I feel there are barriers preventing me from working effectively with the ADHD population |
2.82 (.81) | 2.91 (1.10) | 0.617 |
| Question 6 I feel there are very significant barriers to generalizing treatment for ADHD |
2.57 (.80) | 2.63 (1.11) | 0.752 |
| Question 7 I believe it is possible to generalize treatment outcomes across different settings, people, and behaviors for a child with ADHD. |
2.63 (.89) | 2.08 (.92) | .001* |
| Question 8 I feel that it would be easy to generalize ADHD treatment to multiple environments/settings |
3.08 (.82) | 2.74 (1.15) | 0.055 |
| Question 9 I feel it is important to implement a consistent approach to ADHD in all environments for effective and long-lasting treatment to occur |
1.91(.95) | 1.51 (.62) | .009** |
|
*p < .001, **p<.05 |
|||
As hypothesized, the survey found that professionals who attended the ADHD continuing education conference expressed an increased in their confidence, training, and support of evidence-based treatment approaches for ADHD. Significant differences in pre and post survey outcomes demonstrated a significant increase in perceived importance and willingness of generalizing treatment approaches for ADHD children. For question items 1, 2, 3, 4, 7, 9 there was a significant pre and post conference reporting indicating that within these six domains there was increased training, confidence, support, education of evidence-based treatment, and level of agreement that generalization of ADHD treatment is important. For items 5, 6, and 8 there were no significant differences in pre and post participant measures.
A portion of the survey attempted to capture participant specific barriers to ADHD treatment, through open-ended free response questions. This portion of the survey was not able to be formally analyzed using quantitative measures. The themes worth highlighting from participants who did respond, commented on variables such as “lack of school and administrative support”, “lack of teacher/educator follow through”, “need for improved collaboration between professionals”, “desire to attend additional trainings and continued education”, “increase understanding and application of interventions for clinicians and caregivers in therapy” and lastly, “consistent and appropriate training and supervision for working with ADHD population”.
Discussion
Considering generalization of treatments
Core symptom reduction and functional improvement in the treatment setting is the aim of pharmacologic and psychosocial interventions. Inherent in the ADHD diagnosis, symptoms have direct, negative impacts in multiple settings (e.g., social, academic, home, occupational). Historically, treatment outcomes for ADHD have been suboptimal. Successful ADHD treatment requires symptomatic treatment with pharmacotherapy (stimulants and non- stimulants) and behavioral interventions4 extending to different settings and domains. However, the literature identifies several barriers to the successful management of ADHD resulting in suboptimal outcomes. When discussing successful ADHD treatment, it is important to consider generalization as an essential element. Addressing generalization while treating ADHD provides children and adolescents with increased support and skills to be successful making it an essential component of treatment that requires further discussion. A recent review of Generalization for childhood neurodevelopmental and mental health disorders suggested facilitating long-term treatment gains may be achieved by specifically training for generalization [5].
The findings in response to our research support emerging literature on barriers and factors contributing to ineffective generalization of ADHD treatment. As part of training in a variety of contexts and domains, including caregivers and teachers is implicated in the generalization of therapeutic gains [5]. Although our study provides results that may be helpful within our specific setting and course, it is highly pertinent to the existing literature as it provides a foundation for prospective studies examining outcomes regarding generalization gains of treatments and potential factors contributing to the success. Our study highlights the relevance of extending previous findings aimed to address generalization barriers for ADHD treatment and potential mechanisms underlying treatment impact with the goal of increasing the understanding of sustained symptom change of the ADHD population.
Potential barriers to generalizability
Several factors have been identified as contributing to the difficulty of implementing procedures and focusing on relevant skills to facilitate generalization of ADHD treatments. Inadequate procedures to facilitate treatment generalization (e.g., treatment delivered in only one specific setting) and insufficient foci of treatment (e.g., not targeting specific skills necessary) are identified as potential contributors to variability in treatment generalization [5]. Parents’/caregivers’, teachers’, medical providers’ (e.g., nurses, physicians), or mental health providers’ (e.g., therapists) ability to facilitate generalization may be impacted by beliefs that ADHD will subside on its own, attributing ADHD symptoms to personal characteristics, or that the child’s behavior is solely caused by poor parenting or lack of discipline, beliefs regarding long term side effects of medications, misperceptions regarding duration of treatment, level of engagement in psychosocial treatments, reluctance to use medications, or the opposite, relying solely on medications without psychosocial support, and perception that child’s behavior can be managed on their own [18].
ADHD is also strongly associated with several psychiatric comorbidities According to a 2016 national parent survey of children with ADHD, 6 in 10 children had ADHD and at least one comorbid mental, emotional, or behavioral disorder2 Approximately 52% of children with ADHD had a comorbid behavior or conduct problem, 33% with comorbid anxiety disorder, 17% with comorbid depression and 14% with comorbid autism spectrum disorder [2]. Accurate understanding of the diagnosis and ruling out other diagnoses are both imperative to enhancing treatment and generalization. The American Academy of Pediatrics (AAP) provides guidelines and emphasizes the importance of an accurate ADHD diagnosis in order to ensure and maximize appropriate treatment. However, research indicates that there is limited knowledge among medical providers (primary care physicians, pediatricians) of established AAP guidelines for ADHD treatment [19]. Despite efforts to increase the use of evidence-based treatments, a survey of physician practices indicated only 50% of children with ADHD were receiving care corresponding to practice parameters of the American Academy of Child and Adolescent Psychiatry [20]. Additional salient barriers discussed in the research reveal other medical professionals (e.g., nurses, physicians) experience a lack of confidence in implementing or participating in evidencebased ADHD treatment [21]. Furthermore, the lack of confidence is exacerbated by insufficient training, lack of interest, and/or (dis)comfort with the diagnostic group in general.
Barriers effective ADHD treatment is also recognized by school-based professionals (e.g., teachers, school psychologists,). Teachers report limited knowledge or understanding regarding ADHD-related difficulties and functional implications [22], limiting school-based professionals’ ability to facilitate positive treatment effects in a school setting [23]. In line with these findings and based on pre-conference survey outcomes within this study, a lack of adequate training and education for teachers who work most closely to children with ADHD continue to be a significant barrier to generalizing ADHD treatment.
Addressing barriers
Identified barriers to generalization which are consistent between disciplines previously discussed appear to pertain to (1) confidence in knowledge about ADHD and ADHD treatment and (2) perceptions of barriers to ADHD and ADHD treatment.
A study that further highlights these barriers, conducted by Jane Williams in 2004, reported that 15% of office visits to pediatricians and primary care physicians were for behavioral health disorders with the most frequent being ADD/ADHD [24]. With the onset of ADHD symptoms most commonly occurring in childhood, it is imperative for medical providers have confidence providing treatment as this is often the initial evaluation of children with emotional and behavioral problems [24]. Additionally, symptoms often surface and become impairing in school-based settings as children are required to demonstrate sustained-attention and focus in the classroom, requiring early identification and treatment referrals. As previously discussed, several the barriers recognized by medical and school-based professionals were related to their need for increased education, particularly in the areas of assessment and diagnosis of ADHD and co-morbid disorders. As such, providing information related to the etiology, presentation, and treatment of ADHD and increasing understanding of co-morbid disorders and presentation may be helpful to these disciplines.
For the purposes of this study and the population surveyed, statistical significance for our findings directly relates to a few of the predetermined barrier categories; specifically, assessment and diagnosis, provider and treatment characteristics, and adequate teacher training. Further discussion is outlined in each section below:
Assessment and diagnosis
Based on our findings and conference outcomes, most participants reported significant difference pre and post conference regarding their comfort level and overall reduction of identified barriers. Specifically, participants reported increased comfort utilizing evidence-based treatment for ADHD, increased resources, support and knowledge to work with this population. Accurate assessment and diagnosis require a myriad of external supports, collateral, time and understanding of diagnostic criteria which was shown to improve post conference.
Provider and treatment characteristics
Provider and treatment characteristics are a crucial component to understanding where the potential disparities stem, as the initial point of care is typically with the child’s primary care physician [25]. Identified barriers for providers include: a lack of confidence of implementing or participating in evidence-based treatment by treatment providers (i.e., nurses) and parents of children with ADHD [21] as well as lack of support and resources to implement or seek treatment [20]. The results of the current study indicate that the conference was associated with significant changes in the way participants perceived their level of adequate training and knowledge, confidence in their ability to implement ADHD treatments, and number of resources and support they had, it is possible that future, similar conferences can help address provider specific barriers to treatment generalization.
Teacher training
A major component of our study evaluated whether individuals working with the ADHD population felt they had the support, training, and confidence to work effectively with this population. Specifically, a lack of adequate training and education for those who work most closely to children with ADHD appears to be a significant barrier. Research indicates teachers often exhibit limited knowledge or understanding about the difficulties associated with ADHD and how these difficulties impact the lives of youth with ADHD [22] and shows a need for teachers to receive more training in order to better support children with ADHD [26].
Other studies have further supported the need for additional teacher training working with the ADHD population, supporting our study findings. A study examining the beliefs of children with ADHD, reported that teachers needed to be more knowledgeable of the unique challenges that they face particularly in a school setting to help them improve their performance more effectively in school [23]. Additionally, current research frames gender differences in symptom presentation presents a unique challenge for educators. The symptom variation of ADHD females compared to their male counterparts often result in under identification with female symptoms typically more subtle [27]. This under recognition of females with ADHD has potentially serious academic and public health implications [28,29]. Research suggests providing elementary school teachers and parents with training on recognizing ADHD symptom in both genders and the differential manifestations of the disorder considering diagnosis during the school age is increasingly common due to ADHD symptoms becoming more overt. Within our study, significant changes occurred in post conference ratings regarding support and resources participants felt they had for implementing evidencebased treatments. Participants reported feeling they had more adequate training and education post conference to address ADHD symptom recognition, presentation and interventions.
Strengths and limitations
Our survey and results contribute insights to the perceived barriers related to effective ADHD treatment. Although the treatment barriers are vast, this study provides a framework for how to address the professional and systemic barriers to effective ADHD treatment. While current literature focuses largely on barriers to utilizing evidence-based treatment and specific modalities effectiveness within the ADHD population, professional perception of treatment appears to be an important area of further study. This concept of generalizability is especially important to consider due to the required engagement from professionals and caregivers needed for successful implementation. Unlike other neurodevelopmental diagnoses, which have shown benefit from generalization of treatment, the ADHD population continues to experience salient barriers which prevent long term treatment gains and limited application to non-treatment settings [30].
Overall, the outcomes from the conference in the various areas of statistical significance show the ability for professionals to address perceived barriers through continuing education, training and instruction of evidence-based interventions that span all domains of the ADHD child’s life. Attempts to generalize specific domains, such as social skills, in a vacuum without integration of a systematic evaluation of appropriate interventions have shown ineffective and is unlikely to result in the transference of skills between environments in the absence of active external efforts to promote generalization [31]. Outcomes from this study show trainings and conferences focused on increasing skills and interventions of professionals within the context of generalization show preliminary benefits to address factors related to generalizing ADHD treatment. Although this study had limitations, the results are encouraging and begin to address the foundational changes needed within current ADHD treatment standards.
Our study findings need to be interpreted in the context of several limitations, specifically, convenience sampling, conference specialization, participation rates, and survey limitations. The participants were obtained through convenience sampling in that those eligible for participation in the study were attendees at an ADHD conference put on at the institution. The conference was a highly specialized continuing education opportunity for community professionals, and some community members may not have been able to attend due to financial barriers or limited funding from professional organizations, or geographical proximity, limiting the overall attendance of the conference to only those local individuals who were able to meet the financial obligation. Additionally, the sample size for this study was relatively small and not an adequate representation of the population of providers, school staff and community-based professionals who may interact with children. Although the findings yielded statistically significant results, the findings should be interpreted as preliminary and additional measures with a larger sample size should be conducted. Findings are further limited by participation rates with only 47 of the 70 conference attendees completing the pre and post survey. Lastly, the data collection was limited due to inability to follow up on feedback or to elaborate on responses with specific participants. Even though the survey provided opportunities for open ended survey responses in addition to scale rating questions, the study could have benefitted from better contextualization and additional collateral information from conference attendees. Finally, no data was gathered on clinical practice or change based outcomes following the training.
Conclusion
In conclusion, our study contributes significantly to an area of ADHD research that has limited footing in the current literature. These findings support emerging literature on barriers and factors contributing to ineffective generalization of ADHD treatment. Our multi-perspective survey shows significant changes between pre and post survey outcomes for professionals working with the ADHD population and specific perceived barriers to generalized ADHD treatment. Our findings highlight the need to continue to address generalization barriers to effective treatment and emphasize the importance of engaging professionals working with the ADHD population. Further research must focus on the several barriers to generalization, and exploration of these and other barriers to support changing the standard of care for ADHD treatment. Additionally, developing a standardized content for continuing education for professionals working with the ADHD population focusing on elements of generalizability can assist with capturing specific barriers and factors that may currently be overlooked in the ADHD literature.
Conflicts of Interest
No conflicts of interest and sources of funding for this manuscript.
References
- Homer CJ, Goldberg MJ, Shiffman R, Berger JE, France FL, et al. (2000) clinical practice guideline: Diagnosis and evaluation of the child with Attention-Deficit/Hyperactivity Disorder. Pediatrics 105: 1158-1170.
[Crossref], [Google Scholar]
- clinical practice guideline: Diagnosis and evaluation of the child with Attention-Deficit/Hyperactivity Disorder.
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA, et al. (2007) The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry 164: 942-948.
[Crossref], [Google Scholar], [Indexed]
- Barkley R (2018) Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment book. Guilford Press, New York.
- Swan AJ, Carper MM, Kendall PC (2016) In pursuit of generalization: An updated review. Behav Ther 47: 733-746.
[Crossref], [Google Scholar], [Indexed]
- Abikoff H (2009) ADHD psychosocial treatments: generalization reconsidered.J Atten Disord 13, 207-210.
[Crossref], [Google Scholar], [Indexed]
- Pliszka S (2007) Practice parameter for the assessment and treatment of children and adolescents with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46: 894-921.
[Crossref], [Google Scholar], [Indexed]
- Biederman J, Seidman LJ, Petty CR, Fried R, Doyle AE, et al. (2008) Effects of stimulant medication on neuropsychological functioning in young adults with attention-deficit/hyperactivity disorder.J Clin Psychiatry 69, 1150-1156.
[Crossref], [Google Scholar], [Indexed]
- Barbaresi WJ (1996) Primary-care approach to the diagnosis and management of attention-deficit hyperactivity disorder.Mayo Clin Proc 71: 463-471.
[Crossref], [Google Scholar], [Indexed]
- Chronis AM, Jones HA, Raggi VL (2006) Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder.Clin Psychol Rev 26: 486-502.
[Crossref], [Google Scholar], [Indexed]
- Fabiano GA, Pelham WE, Jr Coles EK, Gnagy EM, Chronis-Tuscano A, et al. (2009) A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder.Clin Psychol Rev 29: 129-140
[Crossref], [Google Scholar], [Indexed]
- Antshel KM, Barkley R (2008) Psychosocial interventions in attention deficit hyperactivity disorder. Child Adolesc Psychiatr Clin N Am 17: 421-437.
[Crossref], [Google Scholar], [Indexed]
- Chronis-Tuscano A, Lewis-Morrarty E, Woods KE, O’Brien KA, Mazursky-Horowitz H, et al. (2016) Parent–Child interaction therapy with emotion coaching for preschoolers with Attention-Deficit/Hyperactivity Disorder. Cogn Behav Pract 23: 62-78.
[Crossref], [Google Scholar]
- McNeil CB, Eyberg S, Eisenstadt TH, Newcomb K, Funderburk B, et al. (1991) Parent–Child interaction therapy with behavior problem children: Generalization of treatment effects to the school setting. J Clin Child Psychol 20 140-151.
[Crossref], [Google Scholar]
- Gallagher R, Abikoff HB, Spira EG (2014) Organizational skills training for children with ADHD: An empirically supported treatment. Guilford Press, New York.
- Gevensleben H, Holl B, Albrecht B, Vogel C, Schlamp D, et al. (2009). Is neurofeedback an efficacious treatment for ADHD? A randomised controlled clinical trial. J Child Psychol Psychiatry 50: 780-789.
[Crossref], [Google Scholar], [Indexed]
- Evans SW, Langberg JM, Egan T, Molitor SJ (2014) Middle school-based and high school-based interventions for adolescents with ADHD. Child Adolesc Psychiatr Clin N Am 23: 699-715.
[Crossref], [Google Scholar], [Indexed]
- Wells KC, Pelham WE, Kotkin RA, Hoza B, Abikoff HB, et al. (2000) Psychosocial treatment strategies in the MTA study: rationale, methods, and critical issues in design and implementation. J Abnorm Child Psychol 28: 483-505.
[Crossref], [Google Scholar], [Indexed]
- Corkum P, Bessey M, McGonnell M, Dorbeck A (2015) Barriers to evidence-based treatment for children with attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord 7: 49-74.
[Crossref], [Google Scholar], [Indexed]
- Miller AR, Johnston C, Klassen AF, Fine S, Papsdorf M (2005) Family physicians' involvement and self-reported comfort and skill in care of children with behavioral and emotional problems: a population-based survey. BMC Fam Pract 6: 12.
[Crossref], [Google Scholar], [Indexed]
- Bussing R, Koro-Ljungberg M, Noguchi K, Mason D, Mayerson G, et al. (2012) Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Soc Sci Med 74: 92-100.
[Crossref], [Google Scholar], [Indexed]
- Frisch L, Moser SE, Hawley F, Johnston J, Romereim M, et al. (2003) Kansas school nurses' knowledge and opinions about ADHD stimulant medication therapy. J Sch Health 73: 127-128.
[Crossref], [Google Scholar], [Indexed]
- Bell L, Long S, Garvan C, Bussing R (2011) The impact of teacher credentials on ADHD stigma perceptions. Psychology in the Schools 48: 184-197.
[Crossref], [Google Scholar]
- Kendall L (2016) ‘The teacher said I'm thick!’ Experiences of children with Attention Deficit Hyperactivity Disorder within a school setting. Support for Learning 31: 122-137
[Crossref], [Google Scholar]
- Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM, et al. (2004) Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics 114 601-606.
[Crossref], [Google Scholar], [Indexed]
- Fremont WP, Nastasi R, Newman N, Roizen NJ (2008) Comfort level of pediatricians and family medicine physicians diagnosing and treating child and adolescent psychiatric disorders. International journal of psychiatry in medicine, 38: 153-168.
[Crossref], [Google Scholar], [Indexed]
- Wheeler L, Pumfrey P, Wakefield P, Quill W (2008) ADHD in schools: prevalence, multi-professional involvements and school training needs in an LEA. Emotional and Behavioural Difficulties 13: 163-177.
[Crossref], [Google Scholar]
- Gershon J (2002) A meta-analytic review of gender differences in ADHD. J Atten Disord 5: 143-154.
[Crossref], [Google Scholar], [Indexed]
- Arnold LE (1996) Sex differences in ADHD: Conference summary. Journal of abnormal child psychology 24: 555-569.
[Crossref], [Google Scholar], [Indexed]
- McGee R, Feehan M (1991) Are girls with problems of attention underrecognized? J Psychopathol Behav Assess 13: 187-198.
[Crossref], [Google Scholar]
- O'Callaghan P, Reitman DM, Northup J, Hupp SD, Murphy MA (2003) Promoting social skills generalization with adhd-diagnosed children in a sports setting. Behavior Therapy 34: 313-330.
[Crossref], [Google Scholar]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences