Problematic Sexual Behavior in a Patient of 48, XXYY Syndrome: A Case Report
Subhash Chandra, Cathryn A Galanter, Kenneth J Weiss and Lenore Engel
DOI10.4172/2472-1786.100018
1University of Pennsylvania, Perelman School of Medicine, USA
2SUNY Downstate / Kings County Hospital Center (KCHC), USA
3SUNY Downstate Medical Center, USA
- *Corresponding Author:
- Subhash Chandra
University of Pennsylvania Perelman School of Medicine, Psychiatry, 3535 Market street Philadelphia, Pennsylvania 19104, USA
Tel: 9178624201
Email: schandra2@yahoo.com
Received Date: January 06, 2016; Accepted Date: February 29, 2016; Published Date: March 07, 2016
Citation: Chandra S, Galanter CA, Weiss KJ, et al. Problematic Sexual Behavior in a Patient of 48, XXYY Syndrome: A Case Report. J Child Dev Disord. 2016, 2:2.doi: 10.4172/2472-1786.100017
Abstract
A 17 year-old-boy with a diagnosis of 48, XXYY syndrome, presented with suicidal ideation and auditory hallucinations. He has had history of problematic sexual behaviors since age six. We discuss his clinical presentation and highlight his behavioral issues, which may be due to low intelligence, sexual abuse, neglect or a behavior pattern of a person with 48, XXYY syndrome. Scientific literature suggests that children at high risk for problematic sexual behavior are those with intellectual disability, history of sexual abuse, neglect, or genetic syndromes. Little is known about the sexual behavior pattern in a case of XXYY syndrome. We discuss this case report to bring forward the sexual presentation of this rare syndrome and how a clinician’s diagnosis-oriented approach fails to address the risky sexual behavior. An important aspect is the lack of training to screen, diagnose, and most importantly intervene optimally.
Keywords
48,XXYY syndrome; Intellectual disability; Schizophrenia; Compulsive sexual behavior
Introduction
48, XXYY is an aneuploidy affecting 1 in 18,000 to 50,000 male births [1]. Patients have delayed dentition and developmental milestones. Endocrine abnormalities include reduced testosterone level, increased follicle stimulating hormone (FSH) and luteinizing hormone (LH) and hypogonadism [2]. Physical characteristics include dysmorphic facial features, elbow abnormalities and poor muscle development. Common medical problems are asthma, peripheral vascular disease, diabetes and intention tremors [3]. The presence of an extra Y chromosome affects neurodevelopment, resulting in developmental delays, learning disabilities, intellectual disabilities, and a spectrum of psychological disorders which differentiates it from Klinefelter syndrome (47, XXY), in which the intellect usually falls in the average range (IQ = 80-120) [4,5]. While there are several reports of co-occurring psychiatric disorders [6] in people with XXYY syndrome, there is no conclusive evidence of increased risk of psychiatric pathology. There are few reports addressing risk taking behavior or sexual impulsivity in 48, XXYY syndrome [7]. We present this case report of a 17 year-old male, who was diagnosed with 48, XXYY syndrome by karyotyping and review the physical and psychological features of people with 48, XXYY. We discuss the problematic sexual behavior in this adolescent which may be due to several factors including his chromosomal abnormality, intellectual impairment, psychiatric disorder or environmental exposures.
Description of the Case Presentation
A 17-year-old African American boy who lived with his maternal step-grandparents was referred by his special education school for psychiatric evaluation after he drew pictures of himself surrounded by fire and guns. His grandmother requested psychiatric admission as she was fearful for him. During evaluation he endorsed suicidal ideation but denied any intent or plan. Grandmother mentioned that he attempted suicide in the past; he stabbed himself with a pen and ran in to traffic once. He did not report any impairment in sleep, concentration and energy. On the Kutcher Adolescent Depression scale (KADS) [8], he scored 4 indicating that he was ‘probably not depressed’. KADS is a self-reported scale specifically designed to diagnose and assess the severity of adolescent depression. We used an abbreviated 6-item scale. 0-5 on the scale is interpreted as probably not depressed; 6 and above is possible depression. He reported hearing voices telling him “to have sex”. He had a delusion of being a “control tower,” whereby he “can make anything happen,” including “changing the world, controlling the water system.” On the Positive and Negative Syndrome Scale (PANSS) [9], he scored 25 out of 49 on positive scale, 15 out of 49 on negative scale, and 28 out of 112 on general psychopathology scale. The PANSS is a 30-item rating scale that is specifically developed to assess individuals with schizophrenia. PANSS is based upon the premises that schizophrenia has two distinct syndromes, a positive and a negative syndrome. Of the 30 items included in the PANSS, 7 constitute a Positive Scale, 7 Negative Scale, and the remaining 16 a General Psychopathology Scale.
He scored high on Sexual Symptom Assessment Scale (S-SAS) [10]. The S-SAS is a 12-item, self-rated scale. It measures severity of symptoms of Compulsive Sexual Behavior (CSB) with each item scored 0–4; higher scores indicate more severe symptoms. He scored 3 on questions such as: ‘How much you were able to control your thoughts of problematic sexual behavior? How much personal trouble or emotional distress the problematic sexual behavior has caused you?’ He scored 4 (constant to near constant) on: ‘How often did thoughts about engaging in problematic sexual behavior come up?’ He reported severe difficulty controlling his urges and thoughts of engaging in problematic sexual behavior. He had severe anticipatory tension / excitement before engaging in such behavior and severe emotional distress and personal trouble caused by his problematic sexual behavior. During his stay in the hospital he never exhibited any impulsive or disruptive behavior. While there were no sexually inappropriate behaviors, he had poor boundaries and tended to stay too close to people. He scored 8 on pervasive developmental disorder rating scale (PDDRS). PDDRS is a behavior rating scale designed to identify individuals potentially meeting criteria for pervasive developmental disorder. It contains 51 items that measure three dimensions: arousal, affect, and cognition. Each item is rated on a five-point Likert scale according to the degree to which the child generally shows the behavior described. The total score is obtained by summing the separate scores for each subscale.
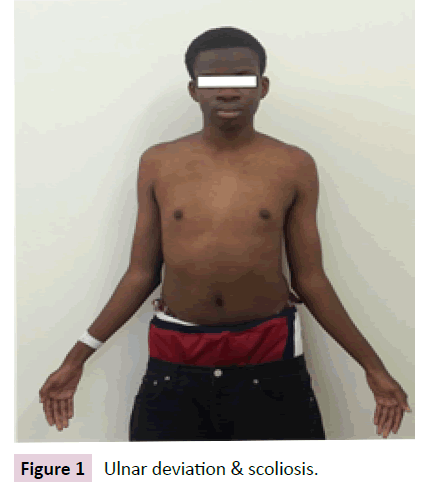
On physical exam, he was a tall boy with atypical facial features; widely set eyes, broad nasal bridge and overcrowding of teeth in both jaws. He had scoliosis and ulnar deviation of both his hands (Figure 1).
Secondary sexual characteristics were fully developed, he was Tanner stage V. He had reduced testicular volume but did not exhibit other hypo gonadal signs such as gynecomastia or scant pubic hair. His EKG showed sinus rhythm, atrial premature complex and left ventricular enlargement with ST elevation. Serum Testosterone level was low normal, 265.80 (241–8270 ng / dl). Levels of both FSH, 21.14 (1.4–18.1 mIU / mL) and LH, 17.02 (1.5–9.3 mIU / ml) were high. His X-ray of the extremities, CT scan of head and rest of the blood tests were unremarkable. He had asthma, asymptomatic for the last 6 years. He had no history of seizures, head trauma or cardiac abnormality.
Past psychiatric history
He received a full developmental evaluation at age 4 and was found to have intellectual disability, attention deficit hyperactive disorder (ADHD), delayed speech and fine motor skills. He received speech and occupational therapy and methylphenidate for ADHD. Methylphenidate was stopped after 2 months, when his grandmother rescinded her consent. Grandmother was of the belief that these medications have “not done any good to any kid. I don’t want to keep my kid drugged.” At age nine, his grandmother took him to a psychiatrist, for inappropriate sexual behavior and episodes of aggression. He was prescribed risperidone (we could not retrieve the treatment details for his treatment provider). He received it for five months with no change in his behavior. He was diagnosed with Asperger’s disorder at age ten at a child development center. In the report available from the development center there is no mention of how and why this diagnosis was given. He did not receive additional psychiatric care until age 16, a year prior to this inpatient admission. He was brought to the emergency room (ER) for suicidal ideation and aggression towards his classmates. He was diagnosed with adjustment disorder with mixed disturbance of emotion and conduct. No psychotropic agents were given and he was discharged with an outpatient follow up appointment. Two days later he returned to the ER, brought by his grandmother because he was hearing voices telling him “to have sex.” He was also having a grandiose delusion that he could make anything happen. He was admitted and diagnosed as having pervasive developmental disorder and brief reactive psychosis. The progress note does not mention the bases for these diagnoses. During the sexual behavior assessment he reported that he was sexually active with multiple partners and watched pornography with his peers. He was first treated with haloperidol, which was discontinued due to extrapyramidal symptoms. He was then started on olanzapine, and after a nineday stay, he was discharged on olanzapine 5 mg for aggression and inappropriate behavior. His grandmother did not want him to take any medication with the belief that “mental medication are no good”. It was later discontinued due to weight gain.
Sexual history
His grandmother first became concerned when he was six years of age and she found him touching his genitals while spying on his female cousin, sister and grandmother while they were changing clothes. She did not seek mental health care at that time. At age 9 he was found performing oral sex on his 2-year-old male cousin. The incident was not reported and there was no Administration of Child Services (ACS) involvement. Grandmother was not sure if it was just a childish behavior or a mental illness. She did not feel the need to report it. He was also touching peers inappropriately at school, and was suspended; since then he has had one-to-one supervision at school. At age 12 he was raped by his 14-year-old male cousin while visiting his mother’s home. The penetration was confirmed by a rape kit. During the same year he was sexually abused on his way home from school by two boys, ages 18 and 15, who made him perform oral sex. At age 14 he was charged for forcing himself on a nine-year-old girl at his mother’s house and performing cunnilingus. He was placed on probation.
Developmental history
While initially in his mother’s custody, at age 4 his grandmother obtained custody due to neglect; she was not aware of any physical or sexual abuse from 0-4 years of age. During a workup for delayed development, genotyping revealed 48, XXYY with CGG repeat sequence unremarkable for Fragile X syndrome. At seven years old his full scale IQ was 70 with verbal IQ of 80 and performance IQ of 65 as measured by WISC-III. When he was ten years old, his Full Scale IQ was 64; verbal IQ was 72, and performance IQ 66 on the WISC III. His adaptive functioning was reported to be consistent with his cognitive functioning. He obtained an adaptive behavior composite of 67, with an age equivalent of seven years and one month. He was reported to be about three years behind his grade at the time of testing. Throughout his record he was described as immature, disruptive, impulsive and inappropriate.
Developmental adversity
His developmental history was significant for being born from a twin pregnancy. He was born full term via C-section. Twin A died of hydrocephalus and encephalitis within 36 hours of birth. His mother suffered from schizophrenia, cocaine dependence, genital herpes, hepatitis C and HIV. She was on psychotropic agent and antiviral medications throughout pregnancy. He was born with HIV antibodies and was on antiretroviral medications for 18 months leading to his seroconversion. He had delayed dentition and speech and started walking at 2 years of age. He developed a peculiar gait, always keeping both his elbows flexed and wrist extended and hands in pronation.
Assessment and plan
IQ testing was not done in the current admission, but results of his psychological tests from last hospitalization were available. He did not meet the criteria for major depressive disorder or schizophrenia. With sudden onset delusions and hallucinations he was given the diagnosis of brief psychotic disorder. To treat his psychotic symptoms, he was started on risperidone which was titrated to one mg each morning and two mg in the evening. He responded well to risperidone and his psychotic symptoms improved. The team discussed with grandmother the option of Juvenile Sex Offenders program. Grandmother did not approve with the idea that “other kids there will make him worse; however, he will gradually get better with time.” Possibility of prescribing Gonadotropin Releasing Hormone agonist was discussed with the team, but because of his age he was not a good candidate. SSRI has shown effectiveness in decreasing the sexual drive, but there is no FDA-approved indication. Finally, with no viable option for treatment of his sexual behavior and not being an imminent danger to self or other, he was discharged to a local mental health clinic. The writer (SC) tried to follow up with the grandmother but she refused to entertain any questions. Rather, she was uncomfortable with the notion that we were trying to address his sexual issues which, according to her, were not very far from normal. She expected him to become normal with time without any need for intervention.
Review of Literature
48, XXYY syndrome, initially considered a variant of Klinefelter syndrome (KS), is a separate chromosomal disorder. It leads to tall stature, long legs, clinodactyly, pes planus and dysmorphic facial feature such as hypertelorism. Patients have high FSH and low plasma testosterone level [6]. They have been diagnosed with tremor, allergies and asthma [11]. Unlike KS which is difficult to diagnose before puberty, XXYY syndrome is diagnosed earlier (on average at 7.7 years of age) due to early developmental delay that are noted from 2nd to 5th year [12]. Autism spectrum [4] disorder and ADHD have been reported in XXYY syndrome [1]. Males with XXYY syndrome often have speech-language disorders, social–emotional difficulties, cognitive impairments, poor visual– perceptual skills and are also more likely to have hyperactive/ impulsive symptoms [4]. The major indication for chromosomal analysis has been mental retardation and behavioral problems, like violent and impulsive reactions [6,13-15]. There have been case reports of children with XXYY presenting with suicidal ideation and aggressive behavior with presumable diagnosis of mixed bipolar episode [16]. In cases presenting with paranoid schizophrenia the psychotic symptoms have gotten worse with testosterone and have not responded to antipsychotics [17]. In XXYY syndrome there is one reported case of sexually abusive behavior, where a cognitive behavioral treatment program was not effective [7].
Research on the sexual development of people with intellectual disabilities (ID) is limited but seems to indicate that people with ID experience the same range of sexual needs and desires as other people [18]. There may be an increase of public masturbation which is thought to be due to their inability to meet their needs in a socially acceptable manner [19].
Case Discussion
Patients with 48, XXYY have low intelligence with poor social and interpersonal skills [17]. They may have behavioral problems such as impulsivity, hyperactivity and bouts of agitation [6]. While there are case reports on medical and psychological problems in patients with XXYY syndrome [14], the literature is limited in regard to their problematic sexual behavior. Through this case report we present sexual behavior in a patient of XXYY syndrome, such as: exhibitionism, voyeurism, fellatio and cunnilingus. His low intellectual functioning also may have played a role in his inability to learn more acceptable ways of handling his sexual desires [20]. However, there is a possibility that there is a different quality to his sexual behavior mediated by his aneuploidy which goes beyond what is seen in mild intellectual disability. These behaviors may also be an outcome of neglect, sexual abuse, impulsivity or psychosis. We undertook to rule out contribution of psychiatric conditions by use of several screening tools. His unsupervised environment may have contributed to repeated sexual exposure and victimization, normalized inappropriate sexual behavior and his not learning societal rules regarding sexual activity.
Conclusion
Patients with XXYY syndrome should be watched closely for any abnormal behavior, especially those which are sexual in nature. Family member’s education and involvement will play a crucial role in supervising these children. Early intervention could address issues of supervision, impulsivity, early trauma and neglect. A structured environment that safeguards children with genetic and intellectual vulnerability and addresses their behavior by teaching coping skills and social norms will be of paramount importance [20]. As with all children and adolescents with developmental or intellectual disabilities, sexual education adapted to their developmental and intellectual level is also thought to be helpful. Active inpatient treatment is warranted if the patient poses threat to self and others. Psychotropic agents can be used to address patient’s aggression or agitation or comorbid conditions. Anecdotally, medications which are known to lower the sexual desire can be tried in adults, but there is no literature for their use in children and adolescents. Further research is needed to understand such behaviors in this patient population.
Consent
The permission for this publication and using the patient’s photograph was obtained from the patient’s grandmother.
Acknowledgement
Special thanks to Dr. Habibur Rahman, and Dr. Kanan Kasturi for their valuable contribution to this case report by giving feedback on the manuscript and collecting all childhood information respectively.
References
- Katulanda P, Rajapakse JR, Kariyawasam J, Jayasekara R, Dissanayake VH, et al. (2012) An adolescent with 48,XXYY syndrome with hypergonadotrophichypogonadism, attention deficit hyperactive disorder and renal malformations. Indian J EndocrinolMetab16:824-826.
- Messina MF, Aversa T, Mami C, Briuglia S, Panasiti I, et al. (2013) Ambiguous genitalia in a 48, XXYY newborn: a casual relationship or a coincidence? JPediatrEndocrinolMetab26:921-923.
- Tartaglia N, Ayari N, Howell S, D’Epagnier C, Zeitler P, et al. (2011) 48, XXYY, 48, XXXY and 49, XXXXY syndromes: not just variants of Klinefelter syndrome. ActaPaediatrica100:851-860.
- Cordeiro L, Tartaglia N, Roeltgen D, Ross J (2012) Social deficits in male children and adolescents with sex chromosome aneuploidy: a comparison of XXY, XYY, and XXYY syndromes. Res DevDisabil 33:1254-1263.
- Khalifa M, Struthers J (2002)Klinefelter syndrome is a common cause for mental retardation of unknown etiology among prepubertal males. Clin Genet 61:49-53.
- Borja-Santos N, Trancas B, Santos Pinto P, Lopes B, Gamito A, et al. (2010) 48,XXYY in a General Adult Psychiatry Department. Psychiatry (Edgmont) 7:32-36.
- Epps KJ (1996)Sexually abusive behaviour in an adolescent boy with the 48,XXYY syndrome: a case study. CrimBehavMent Health 6:137-146.
- LeBlanc JC, Almudevar A, Brooks SJ, Kutcher S (2002) Screening for adolescent depression: comparison of the Kutcher Adolescent Depression Scale with the Beck Depression Inventory.J Child AdolescPsychopharmacol12:113-126.
- Kay SR, Flszbein A, Opfer LA (1987)The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13:261.
- Raymond NC, Lloyd MD, Miner MH, Kim SW (2007) Preliminary report on the development and validation of the Sexual Symptom Assessment Scale. Sexual Addiction & Compulsivity 14:119-129.
- Lote H, Fuller GN, Bain PG (2013) 48, XXYY syndrome associated tremor. Practical neurology 13:249-253.
- Visootsak J, Ayari N, Howell S, Lazarus J, Tartaglia N, et al. (2013) Timing of diagnosis of 47, XXY and 48, XXYY: A survey of parent experiences. Am J Med Genet A Part A 161:268-272.
- Borghgraef M, Fryns JP, Van den Berghe H (1991) The 48,XXYY syndrome. Follow-up data on clinical characteristics and psychological findings in 4 patients.Genet Couns2:103-108.
- Tartaglia N, Davis S, Hench A, Nimishakavi S, Beauregard R, et al. (2008) A new look at XXYY syndrome: Medical and psychological features. Am J Med Genet A Part A 146A:1509-1522.
- Sørensen K, Nielsen J, Jacobsen P,Rølle T (1978) The 48, XXYY syndrome. Journal of mental deficiency research.
- Lolak S, Dannemiller E, Andres F (2005) 48, XXYY syndrome, mood disorder, and aggression.Am J Psych 162:1384-1384.
- Lee JW (1996) An XXYY male with schizophrenia.Australasian and NZ Jof Psychiatry30:553-556.
- Eastgate G (2008) Sexual health for people with intellectual disability. SaludPublicaMex50 Suppl 2:s255-259.
- Hellemans H, Roeyers H, Leplae W, Dewaele T, Deboutte D, et al. (2010) Sexual behavior in male adolescents and young adults with autism spectrum disorder and borderline/mild mental retardation. Sex Disabil28:93-104.
- Ward T, Beech A (2006)An integrated theory of sexual offending. Aggress Violent Behav11:44-63.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences